
Pandangan Terperinci pada Pembedahan Epilepsi
09 Oct, 2023
 Pasukan Healthtrip
Pasukan HealthtripEpilepsy surgery is a beacon of hope for those dealing with persistent seizures despite medication. For some, it's a transformative option, promising better seizure control and an improved quality of life. This journey explores the ins and outs of epilepsy surgery, from the first evaluation to the latest breakthroughs. It's about empowering individuals and building confidence in the potential of this surgical intervention to make a positive difference.
Ubah Kecantikan Anda, Tingkatkan Keyakinan Anda
Cari kosmetik yang betul prosedur untuk keperluan anda.

Kami pakar dalam pelbagai jenis daripada prosedur kosmetik

Indications for Epilepsy Surgery
- Failed response to medications
- Identification of a specific, treatable cause
- Seizures originating in a single, well-defined area of the brain
- Impact on daily life and quality of life
Types of Epilepsy Surgery
Epilepsy surgery encompasses various procedures aimed at mitigating or eliminating seizures. The choice of surgery depends on factors such as the location of the seizure focus, the individual's overall health, and the nature of the seizures. Here are several types of epilepsy surgeries:
- Temporal Lobectomy:
- Removal of a portion of the temporal lobe, a common site for seizure origin.
- Effective for individuals with temporal lobe epilepsy and a well-defined seizure focus in that region.
- Frontal Lobectomy:
- Surgical removal of a portion of the frontal lobe.
- Suitable for cases where seizures originate in the frontal lobe and are not responsive to medications.
- Multiple Subpial Transection:
- Interrupting nerve fibers without removing brain tissue, preserving important functions while preventing the spread of seizures.
- Applied when the seizure focus is located in areas critical for speech, motor function, or sensory processing.
- Corpus Callosotomy:
- Severing the corpus callosum, the bundle of nerve fibers connecting the brain's hemispheres, to prevent the spread of seizures between hemispheres.
- Considered for individuals with severe and uncontrollable generalized seizures.
- Vagus Nerve Stimulation (VNS):
- Implantation of a device that stimulates the vagus nerve at regular intervals to reduce seizure frequency.
- Indication: Used for individuals with medically refractory epilepsy and those not suitable for resective surgery.
- Responsive Neurostimulation (RNS):
- Implanting a device that monitors brain activity and delivers targeted electrical stimulation to interrupt the onset of seizures.
- Suitable for focal epilepsy when the precise seizure focus is identified.
- Laser Interstitial Thermal Therapy (LITT):
- Minimally invasive procedure using laser energy to heat and destroy abnormal brain tissue causing seizures.
- Applied when the seizure focus is in an area that is challenging to access with traditional open surgery.
Before Surgery:
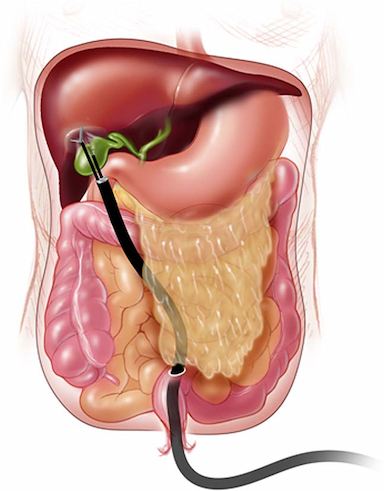
Prosedur paling popular dalam
Laparoskopi Cystecto
Diskaun sehingga 80%.
90% Dinilai
Memuaskan
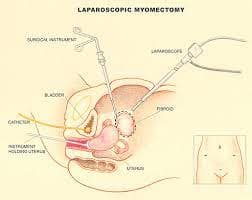
Miomektomi Laparosko
Diskaun sehingga 80%.
90% Dinilai
Memuaskan

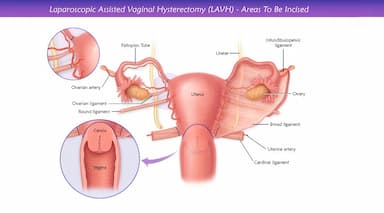
Lavh
Diskaun sehingga 80%.
90% Dinilai
Memuaskan
CATATAN
Diskaun sehingga 80%.
90% Dinilai
Memuaskan
CABG
Diskaun sehingga 80%.
90% Dinilai
Memuaskan
- Preoperative Evaluation:
- Neurological Assessment: A thorough neurological examination is conducted to evaluate the nature and frequency of seizures, as well as their impact on daily life.
- Psychiatric Evaluation: Patients undergo psychiatric assessment to address any mental health concerns that may impact surgery and recovery.
- Cardiovascular and Pulmonary Assessment: Comprehensive evaluation of cardiovascular and pulmonary function to ensure the patient is fit for surgery.
- Imaging Studies:
- High-Resolution MRI: Utilizing high-resolution MRI, neurosurgeons can precisely visualize brain structures and identify abnormalities associated with epilepsy.
- Functional MRI (fMRI): Functional MRI is employed to map brain function and identify critical areas such as those controlling speech and motor function.
- Diffusion Tensor Imaging (DTI): DTI helps map the brain's white matter tracts, providing information about connectivity and aiding surgical planning.
- Advanced EEG Monitoring:
- Long-term Video EEG Monitoring: Continuous monitoring over several days allows for the recording and analysis of seizure patterns, providing critical information for surgical planning.
- Magnetoencephalography (MEG): MEG measures the magnetic fields produced by neural activity, aiding in localizing the source of epileptic activity with high spatial accuracy.
- Neuropsychological Testing:
- Memory and Cognitive Testing: Detailed assessments to evaluate memory, language, and cognitive functions, ensuring a comprehensive understanding of the patient's baseline abilities.
- Invasive Monitoring (if needed):
- Intracranial EEG (icEEG): In some cases, electrodes may be implanted directly into the brain for more precise monitoring of seizure activity.
During Surgery:
- Anesthesia and Monitoring:
- Advanced Anesthesia Techniques: Anesthesia is administered by an experienced anesthesiologist, employing advanced techniques to ensure a controlled and safe environment.
- Continuous Monitoring: Intraoperative monitoring includes EEG, evoked potentials, and other measures to track brain function in real-time.
- Minimally Invasive Approaches:
- Laser Interstitial Thermal Therapy (LITT): Minimally invasive laser therapy may be used for precise ablation of seizure foci, reducing the need for extensive craniotomy.
- Robot-Assisted Surgery: Robotics can assist surgeons in performing more precise procedures with minimal invasiveness.
- Responsive Neurostimulation (RNS):
- Implantation of RNS Device: In cases where traditional resection is not possible, a neurostimulation device may be implanted to detect and respond to abnormal brain activity, modulating neural circuits.
- Advanced Imaging Guidance:
- Intraoperative MRI (iMRI): Real-time MRI during surgery allows for dynamic imaging, enhancing the surgeon's ability to navigate and confirm the extent of resection.
After Surgery:
- Intensive Care and Monitoring:
- ICU Care: Postoperative care begins in the intensive care unit, with continuous monitoring of vital signs and neurological status.
- Early Mobilization: Encouraging early mobilization to reduce the risk of complications such as blood clots.
- Postoperative Imaging and Validation:
- Postoperative MRI and CT Scan: Imaging studies are conducted to assess the success of the surgery and identify any complications.
- Validation of Resection: Neuropsychological testing is performed postoperatively to validate the resection's impact on cognitive and memory functions.
- Medication Adjustment:
- Antiepileptic Drugs (AEDs): Gradual adjustment of AEDs based on postoperative seizure control and individual patient response.
- Rehabilitation and Follow-up:
- Physical and Occupational Therapy: Tailored rehabilitation programs to address motor function, coordination, and activities of daily living.
- Speech Therapy: If applicable, speech therapy is initiated to address any language-related issues.
Latest Advancements:
- Genomic and Precision Medicine:
- Genomic Profiling: Genetic testing to identify specific genetic factors influencing epilepsy, allowing for targeted and personalized treatment approaches.
- Neurostimulation Innovations:
- Closed-Loop Neurostimulation: Advancements in closed-loop systems that can adaptively modulate stimulation based on real-time brain activity patterns.
- Artificial Intelligence in Surgical Planning:
- AI-Based Surgical Planning: Utilizing artificial intelligence algorithms to analyze imaging data and optimize surgical planning for greater precision.
- Brain-Computer Interfaces (BCIs):
- BCIs for Rehabilitation: Exploring the use of BCIs to enhance postoperative rehabilitation and restore function through brain-machine interfaces.
Risks and Complications
- Infection:
- Strict adherence to aseptic techniques during surgery.
- Prophylactic antibiotics administered before surgery as appropriate.
- Bleeding:
- Careful control of bleeding during the surgical procedure.
- Monitoring of blood clotting factors and platelet levels.
- Neurological Deficits:
- Precision in surgical techniques to minimize damage to surrounding brain tissue.
- Real-time monitoring of neurological function during surgery.
- Cognitive and Memory Changes:
- Thorough preoperative neuropsychological assessments to establish baseline cognitive function.
- Tailoring surgical approaches to minimize impact on memory-related structures.
Strategies to Prevent Complications
- Comprehensive Preoperative Evaluation:
- Thorough assessment of the patient's overall health and any pre-existing conditions.
- Informed and Shared Decision-Making:
- Open communication between the healthcare team and the patient regarding potential risks.
- Active involvement of the patient in decision-making processes
- Use of Advanced Imaging Techniques:
- Utilization of advanced imaging modalities for precise surgical planning.
- Minimization of the surgical area to reduce potential impact on non-seizure-related brain regions.
- Postoperative Monitoring and Care:
- Intensive care in the immediate postoperative period to detect and address complications early.
- Regular follow-up appointments to monitor long-term outcomes and address emerging issues.
- Patient Education and Compliance:
- Thorough education of the patient on postoperative care instructions.
- Encouragement of compliance with medications, rehabilitation programs, and lifestyle adjustments.
In concluding our exploration of epilepsy surgery, we recognize its power to redefine lives. Success stories underscore not only seizure control but the restoration of independence and improved quality of life. With ongoing advancements promising refined approaches, epilepsy surgery stands as a testament to resilience and dedicated healthcare, envisioning a future where its transformative impact continues to shine brightly.
Rawatan Kesihatan
Beri diri anda masa untuk berehat
Harga Terendah Dijamin!

Harga Terendah Dijamin!
