
Au-delà du tabou : faire la lumière sur le cancer de la vulve
12 Oct, 2023
 Équipe Healthtrip
Équipe HealthtripVulvar cancer, an uncommon but impactful malignancy, originates in the external female genitalia. This includes the labia, clitoris, and vaginal opening. Predominantly of the squamous cell carcinoma type, it poses unique challenges for affected individuals. This brief overview sets the stage for an exploration into the types, symptoms, causes, and treatments associated with vulvar cancer, aiming to enhance our understanding of this complex and often overlooked condition.
Transformez votre beauté, Boostez votre confiance
Trouver le bon cosmétique procédure adaptée à vos besoins.

Nous sommes spécialisés dans une large gamme des procédures cosmétiques

Types of Vulvar Cancer
A. Squamous Cell Carcinoma
Squamous cell carcinoma is the most common type of vulvar cancer, accounting for a significant majority of cases. It typically originates in the thin, flat cells lining the surface of the vulva.
B. Adenocarcinoma
Adenocarcinoma is a less common form of vulvar cancer, arising from the glandular cells in the vulva. While less prevalent, it presents distinct challenges in diagnosis and treatment compared to squamous cell carcinoma.
C. Melanoma
Melanoma of the vulva is a rare but potentially aggressive form of cancer that develops from the pigment-producing cells (melanocytes). It often requires specialized care due to its unique characteristics and behavior.
Procédures les plus populaires dans
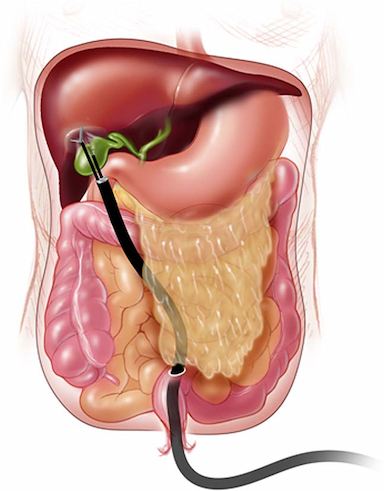
Cystectomie laparosc
Jusqu'à 80% de réduction
Noté à 90 %
Satisfaisant
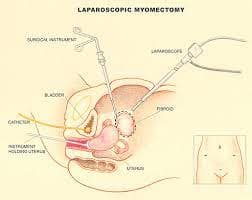
Myomectomie laparosc
Jusqu'à 80% de réduction
Noté à 90 %
Satisfaisant

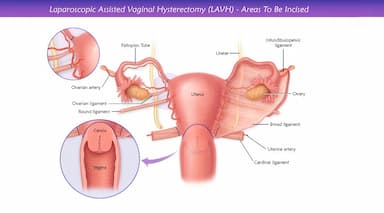
LAVH
Jusqu'à 80% de réduction
Noté à 90 %
Satisfaisant
NOTE
Jusqu'à 80% de réduction
Noté à 90 %
Satisfaisant
PAC
Jusqu'à 80% de réduction
Noté à 90 %
Satisfaisant
Symptoms and Signs
The symptoms and signs of vulvar cancer are important to recognize for early detection and prompt treatment. Common symptoms include:
- Itching or Burning: Persistent itching or burning sensations in the vulvar area are often one of the first symptoms noticed.
- Pain: Women may experience pain or discomfort in the vulvar region, especially when urinating or during intercourse.
- Skin Changes: Changes in the skin of the vulva, such as thickening, color changes (red or white areas), or the presence of a rash or warts.
- Lump or Growth: A lump, growth, or ulcer on the vulva that doesn't heal can be a sign of vulvar cancer.
- Bleeding or Discharge: Unusual vaginal bleeding or discharge not related to menstruation can be a symptom.
- Tenderness: The vulvar area may become tender or swollen.
- Open Sores: Persistent or recurrent ulcers or sores on the vulva that do not heal within a few weeks.
- Change in Skin Texture: The skin around the vulva may become rougher or thicker.
Causes
- HPV Infection: A significant cause of vulvar cancer is infection with certain types of human papillomavirus (HPV), especially strains HPV-16 and HPV-18. These strains can cause cellular changes in the vulva, leading to cancer.
- Aging: The risk of vulvar cancer increases with age, particularly in women over 50 years old. This is partly due to the cumulative effect of other risk factors over time.
- Smoking: Tobacco use is linked to an increased risk of vulvar cancer. Smoking affects the immune system and its ability to fight off infections like HPV, which can lead to cancerous changes in vulvar cells.
- Lichen Sclerosus: This chronic skin condition causes thin, patchy areas of skin, usually on the vulva. While benign, it can increase the risk of vulvar cancer.
- Immunosuppression: Women with weakened immune systems, whether due to conditions like HIV/AIDS or to immunosuppressive medications taken after organ transplants, are at a higher risk.
- Skin Conditions: Chronic or long-standing dermatological conditions affecting the vulva, such as eczema or psoriasis, may increase the risk of developing vulvar cancer.
Diagnosis
A. Physical Examination
A thorough physical examination by a healthcare professional is often the initial step in diagnosing vulvar cancer. This examination may include a visual inspection of the vulva, palpation of the area, and assessment of any abnormalities or unusual symptoms reported by the patient.
B. Biopsy
A biopsy is a critical diagnostic procedure wherein a small sample of tissue is collected from the vulvar area for laboratory analysis. This helps confirm the presence of cancer, identify its type, and determine its characteristics, such as the degree of aggressiveness.
C. Imaging Tests (CT, MRI)
Imaging tests, such as computed tomography (CT) scans and magnetic resonance imaging (MRI), may be employed to assess the extent of cancer, determine if it has spread to nearby tissues or lymph nodes, and aid in the overall staging of the disease. These tests provide valuable information to guide treatment planning.
Treatment
A. Surgery
Surgery is a primary treatment modality for vulvar cancer. The extent of surgery depends on factors such as the size and stage of the tumor. Procedures may include:
- Wide Local Excision: Removal of the tumor and a margin of surrounding healthy tissue.
- Vulvectomy: Partial or complete removal of the vulva.
- Lymph Node Dissection: Removal of nearby lymph nodes to check for the spread of cancer.
B. Radiation Therapy
Radiation therapy uses high-energy rays to target and destroy cancer cells. It is often employed after surgery to eliminate any remaining cancer cells or as a primary treatment in cases where surgery may not be suitable. External beam radiation or brachytherapy (internal radiation) may be used.
C. Chemotherapy
Chemotherapy involves the use of drugs to kill or slow the growth of cancer cells. It may be administered orally or intravenously. Chemotherapy is often employed in cases where cancer has spread beyond the vulva or when there is a high risk of recurrence.
D. Immunotherapy
Immunotherapy is a newer approach that stimulates the body's immune system to recognize and attack cancer cells. While not yet a standard treatment for all vulvar cancers, ongoing research is exploring the potential of immunotherapy in specific cases, especially for advanced or recurrent disease.
Risk Factors
1. HPV Infection: A significant risk factor for vulvar cancer is infection with certain types of human papillomavirus (HPV), particularly HPV-16 and HPV-18.
2. Age: The risk of developing vulvar cancer increases with age, with most cases diagnosed in women over the age of 50.
3. Smoking: Tobacco use has been linked to an increased risk of vulvar cancer, as smoking affects the immune system's ability to fight off HPV infections.
4. Lichen Sclerosus: This skin condition, which causes thin, white patches of skin, usually in the genital area, can increase the risk of vulvar cancer.
5. Immunosuppression: Individuals with weakened immune systems, such as those with HIV/AIDS or those taking immunosuppressive drugs after organ transplants, are at a higher risk.
6. Skin Conditions: Chronic or long-term skin conditions affecting the vulva, such as eczema or psoriasis, may increase the risk.
6. History of Cervical or Vaginal Pre-cancer: Women who have had cervical or vaginal pre-cancer (dysplasia) are at a higher risk of developing vulvar cancer.
Complications
1. Local Spread of Cancer: Vulvar cancer can extend to nearby areas such as the vagina, anus, and urethra, complicating treatment and prognosis.
2. Lymphedema: After surgery or radiation, lymphatic fluid may accumulate in the legs or groin, causing painful swelling.
3. Sexual Dysfunction: Treatments can affect sexual function, libido, and body image, impacting sexual health and intimacy.
4. Chronic Pain: Long-term pain, especially in the pelvic area or during intercourse, can result from treatments.
5. Psychological Impact: The emotional toll of dealing with vulvar cancer can include anxiety, depression, and stress.
These complications highlight the importance of comprehensive care, including physical and emotional support, for those undergoing treatment for vulvar cancer.
Prevention
Prevention strategies for vulvar cancer focus on reducing risk factors and early detection of precancerous conditions. Here are some key preventive measures:
- HPV Vaccination: Since certain types of human papillomavirus (HPV) are linked to vulvar cancer, getting vaccinated against HPV can significantly reduce the risk.
- Regular Screening and Pap Tests: Regular pelvic exams and Pap tests can help detect changes in the vulva that might indicate precancerous conditions or early stages of cancer.
- Safe Sexual Practices: Using barrier methods during sex, such as condoms, can reduce the risk of HPV infection.
- Avoiding Tobacco Use: Smoking is a known risk factor for vulvar cancer. Quitting smoking can lower the risk.
- Maintaining a Healthy Immune System: A strong immune system can fight off HPV infections. This can be achieved through a balanced diet, regular exercise, and adequate sleep.
- Prompt Treatment of Pre-cancerous Conditions: Treating vulvar intraepithelial neoplasia (VIN), a precancerous condition, can prevent the development of vulvar cancer.
- Monitoring and Self-Examination: Regular self-examination of the vulvar area for any changes or abnormalities, and reporting them to a healthcare provider, can lead to early detection and treatment.
These preventive measures are particularly important for individuals at higher risk due to factors like a history of HPV infection or immunosuppression.
Outlook/Prognosis
- Stage at Diagnosis:
- The prognosis for vulvar cancer is influenced by the stage at which it is diagnosed. Early detection, often at an initial stage, generally yields a more favorable prognosis.
- Response to Treatment:
- The effectiveness of treatment plays a crucial role in determining the prognosis. Timely and comprehensive interventions, such as surgery, radiation, and chemotherapy, contribute to positive outcomes.
- Follow-up Care:
- Ongoing monitoring and follow-up care are essential post-treatment. Regular check-ups, imaging tests, and assessments help detect and address any potential recurrence or complications.
In conclusion, vulvar cancer is a complex and relatively rare malignancy that requires a multidimensional approach for effective management. Early detection through vigilant monitoring of symptoms, coupled with timely and appropriate treatment, significantly impacts the prognosis. The integration of preventive measures, such as vaccination and lifestyle changes, is pivotal in reducing risk. As research continues to advance, the understanding of vulvar cancer will evolve, offering hope for improved outcomes and quality of life for those affected by this condition.
Soins de bien-être
Donnez-vous le temps de vous détendre
Prix les plus bas garantis !

Prix les plus bas garantis !



