
A Closer Look at Oral Cancer Surgery
09 Oct, 2023
 Rajwant Singh
Rajwant SinghThis blog aims to provide a balanced exploration of oral cancer, beginning with an overview of the condition and its various types. Moving forward, the focus will shift to the role of oral cancer surgery, objectively examining its significance in the overall treatment landscape and its integration with other therapeutic approaches. The intent is to offer a comprehensive understanding without sensationalism, shedding light on the medical intricacies associated with oral cancer and its surgical interventions.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Indications and Candidates for Oral Cancer Surgery
Conditions Requiring Surgery
- Tumor Size and Stage:
- In certain cases of oral cancer, the size and stage of the tumor become crucial factors in determining the need for surgery. Larger tumors or those in advanced stages may necessitate surgical intervention to effectively manage and address the condition.
- Spread to Surrounding Tissues:
- When oral cancer extends beyond its initial site and invades surrounding tissues, surgery may be recommended. Removing cancerous cells from affected areas helps prevent further progression and improves the chances of successful treatment.
- Lymph Node Involvement:
- Lymph nodes play a pivotal role in the spread of cancer. If oral cancer is detected in the lymph nodes, surgical procedures may be employed to remove affected nodes and control the disease's progression.
Who Need Oral Cancer Surgery ?
- Candidates Based on Diagnosis:
- Individuals diagnosed with oral cancer become potential candidates for surgery, particularly when the condition meets specific criteria such as tumor size, stage, and lymph node involvement. Surgical interventions are tailored to each patient's unique circumstances, with the goal of achieving optimal outcomes.
- Importance of Early Detection:
- Emphasizing the significance of early detection cannot be overstated. Detecting oral cancer in its initial stages increases the likelihood of successful treatment and minimizes the extent of surgery required. Regular screenings and prompt medical attention significantly contribute to better prognoses for patients.
Pre-Surgery Procedures
Diagnosis and Staging
- Biopsy and Pathology:
- The cornerstone of diagnosing oral conditions, including cancer, lies in a biopsy. Tissue samples are collected and analyzed by pathologists to determine the presence of abnormal cells. This crucial step guides healthcare professionals in formulating an accurate diagnosis and tailoring subsequent treatment plans accordingly.
- Imaging Studies (MRI, CT Scans):
- Complementing the insights gained from biopsies, imaging studies such as Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans contribute valuable information about the extent of the disease. These diagnostic tools aid in staging, allowing healthcare providers to assess the size of tumors and identify potential spread to adjacent structures.
Preparing the Patient
Most popular procedures in India
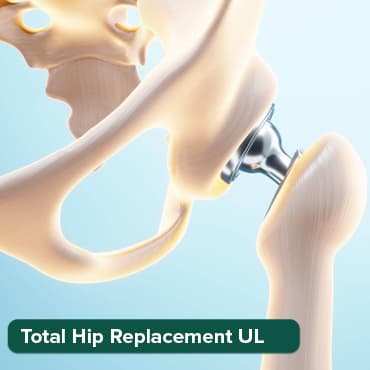
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
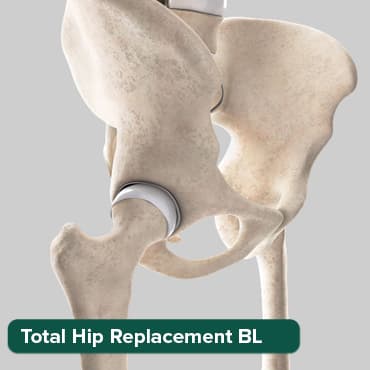
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ANGIOGRAM
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

- Physical Evaluation:
- Before embarking on any surgical intervention, a thorough physical evaluation is conducted. This involves assessing the patient's overall health, identifying potential risk factors, and ensuring that the individual is physically prepared for the upcoming procedure. Addressing pre-existing health conditions is crucial to enhance the patient's resilience during surgery.
- Psychological Preparation:
- Recognizing the emotional impact of a cancer diagnosis is integral to holistic patient care. Psychological preparation involves providing information about the upcoming surgery, discussing potential outcomes, and addressing any concerns the patient may have. Creating an open dialogue fosters a supportive environment and aids in alleviating anxiety associated with the surgical process.
- Informed Consent Process:
- An essential component of patient autonomy and ethical medical practice, the informed consent process ensures that individuals are fully aware of the risks, benefits, and alternatives associated with the proposed surgery. This transparent communication empowers patients to make informed decisions about their treatment and fosters a collaborative relationship between healthcare professionals and patients.
Oral Cancer Surgery Procedure
A.Surgical Techniques
- Tumor Resection:
- Tumor resection involves the precise removal of oral cancer, focusing on preserving healthy tissues. It is tailored based on tumor characteristics like size and location to optimize cancer removal.
- Neck Dissection:
- Neck dissection removes affected lymph nodes in the neck to prevent cancer spread. The extent varies based on lymph node involvement, addressing the specific needs of each patient.
- Reconstruction Procedures:
- Reconstruction aims to restore oral function post-surgery. Techniques include grafts or flaps to rebuild structures, improving the patient's ability to speak and swallow.
B. Anesthesia and Monitoring
1. Types of Anesthesia Used:
- Anesthesia choices—local, regional, or general—are tailored to the surgery's nature and duration, optimizing patient comfort and safety.
- Continuous monitoring of vital signs (heart rate, blood pressure, oxygen levels) ensures patient safety during surgery. Specialized monitors identify and address potential complications promptly.
Post-Surgery Recovery and Care
A. Immediate Postoperative Period
- Monitoring Vital Signs:
- Immediate postoperative care involves vigilant monitoring of vital signs such as heart rate, blood pressure, and oxygen levels. This continuous assessment ensures early detection of any potential complications and allows for prompt intervention, contributing to the patient's safety and recovery.
- Pain Management:
- Effectively managing postoperative pain is essential for the patient's comfort and recovery. Pain management strategies may include medications, patient-controlled analgesia (PCA), or other modalities tailored to the individual's needs. Adequate pain control is pivotal for facilitating early mobilization and optimizing the healing process.
B. Rehabilitation
- Speech Therapy:
- Speech therapy plays a crucial role in the rehabilitation process, especially if the surgery has impacted vocal structures. Speech therapists work with patients to address speech difficulties, improve articulation, and enhance communication skills. This rehabilitation aims to restore and maximize the patient's ability to express themselves effectively.
- Swallowing Rehabilitation:
- Postoperative changes, especially after oral cancer surgery, may affect swallowing function. Swallowing rehabilitation, often guided by speech therapists or swallowing specialists, focuses on retraining and strengthening the muscles involved in swallowing. This ensures a gradual and safe return to normal swallowing function.
C. Long-Term Recovery
- Follow-Up Appointments:
- Long-term recovery involves a structured schedule of follow-up appointments with healthcare providers. These appointments allow for the monitoring of the patient's overall health, evaluation of recovery progress, and addressing any emerging concerns or complications. Regular follow-ups are crucial for optimizing long-term outcomes.
- Surveillance for Recurrence:
- Continued surveillance for cancer recurrence is a key component of long-term recovery. Periodic imaging studies, physical examinations, and other diagnostic tools help healthcare professionals monitor for any signs of cancer recurrence. Early detection of recurrence enhances the effectiveness of subsequent interventions, if needed.
Latest Advancements in Oral Cancer Surgery
A. Robotic Surgery
- Overview of Robotic-Assisted Procedures:
- Robotic surgery involves advanced technology where a surgeon controls a robot to perform precise procedures. This minimally invasive approach allows for enhanced precision and flexibility, often used in various surgical fields, including oral cancer procedures.
- Benefits and Limitations:
- Benefits include smaller incisions, reduced blood loss, and quicker recovery times. The robot's dexterity allows for intricate maneuvers. However, limitations may include cost and the need for specialized training. Not all procedures are suitable for robotic assistance.
B. Immunotherapy
- Role in Post-Surgery Treatment:
- Immunotherapy is a post-surgery treatment that harnesses the body's immune system to target and destroy cancer cells. It complements surgery by addressing residual cancer cells and preventing recurrence. This approach aims to enhance the body's natural defenses against cancer.
- Impact on Outcomes: Immunotherapy has shown promising results in improving long-term outcomes. By boosting the immune response, it may enhance the body's ability to fight cancer. However, individual responses can vary, and ongoing research aims to refine its effectiveness in different cancer scenarios.
Tips for Preparing Yourself
A. Mental and Emotional Preparation
- Support Systems:
- Be in network of family, friends, and healthcare professionals.
- Seek emotional support through support groups or counseling.
- Foster open communication with loved ones about your feelings and concerns.
- Coping Strategies:
- Learn and practice relaxation techniques, such as deep breathing or meditation.
- Develop positive coping mechanisms like journaling or engaging in hobbies.
- Consider professional counseling to navigate emotional challenges.
B. Physical Preparation
- Pre-Surgery Fitness:
- Engage in low-impact exercises to improve overall fitness.
- Consult with healthcare providers for appropriate pre-surgery physical activities.
- Focus on activities promoting flexibility and strength.
- Nutrition Guidelines:
- Follow a balanced diet rich in vitamins and nutrients.
- Ensure adequate hydration before surgery.
- Consult with a nutritionist for personalized dietary recommendations.
Surgical Risks
- Bleeding:
- Potential for postoperative bleeding, which may require additional intervention.
- Risk influenced by factors such as clotting disorders or blood-thinning medications.
- Infection:
- Risk of infection at the surgical site or in the surrounding areas.
- Precautions include proper sterilization protocols and antibiotic administration.
- Nerve Damage:
- Possibility of damage to nerves during surgery, impacting sensation or function.
- Surgeons employ precision techniques to minimize this risk, but it remains a consideration.
B. Strategies to Prevent Complications
- Preoperative Screenings:
- Thorough screenings before surgery to identify and address potential risk factors.
- Assessments include medical history, laboratory tests, and imaging studies.
- Surgical Techniques to Minimize Risks:
- Precision surgical techniques to minimize bleeding and reduce the risk of complications.
- Use of advanced technology and imaging during surgery for enhanced precision.
Factors Influencing Prognosis
A. Outlook and Prognosis
- Stage of Cancer:
- The stage at which oral cancer is diagnosed significantly influences the prognosis.
- Advanced stages may present more challenges in treatment and long-term outcomes.
- Response to Treatment:
- The effectiveness of the chosen treatment plan, including surgery and subsequent therapies, directly impacts prognosis.
- Positive response enhances the likelihood of improved long-term outcomes.
B. Quality of Life After Surgery
- Impact on Speech and Eating:
- Oral cancer surgery may affect speech and eating initially.
- Rehabilitation and support play key roles in adapting to any changes for an improved quality of life.
- Rehabilitation Outcomes:
- Rehabilitation efforts post-surgery influence the overall quality of life.
- Successful rehabilitation enhances functionality and aids in restoring a sense of normalcy.
In short, prognosis is influenced by cancer stage and treatment response, while post-surgery, the focus is on adapting to changes in speech and eating through effective rehabilitation for an improved quality of life.
Oral cancer surgery is crucial for tumor removal and disease management, playing a vital role in treatment success. The holistic approach, integrating surgery with psychological and rehabilitative aspects, is essential for comprehensive care and optimal outcomes.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!







