
LVAD: A Lifesaving Breakthrough in Cardiac Care
12 Nov, 2023
 Healthtrip
HealthtripIntroduction
The human heart is a remarkable organ, responsible for pumping oxygen-rich blood throughout the body. However, when the heart is weakened due to various cardiac conditions, it struggles to perform this crucial function, leading to heart failure. In such cases, medical science has made significant strides in recent years, with one remarkable advancement being the Left Ventricular Assist Device (LVAD). This groundbreaking technology serves as a lifeline for individuals with severe heart failure and has transformed the landscape of cardiac care.
What is an LVAD?
A Left Ventricular Assist Device, often referred to as an LVAD, is a mechanical pump designed to assist the left ventricle of the heart in pumping blood. It is surgically implanted in patients who are experiencing end-stage heart failure or who have a severely weakened heart muscle, making it difficult for the heart to meet the body's oxygen and nutrient demands.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Components of an LVAD (Left Ventricular Assist Device)
1. Pump
The core component of the LVAD is the pump. This pump is responsible for drawing blood from the left ventricle of the heart and then pumping it into the aorta, effectively assisting the heart's function. The pump is a vital part of the LVAD that ensures blood circulation.
2. Power Source
LVADs are typically powered by an external controller and battery pack. These components provide the necessary energy to operate the LVAD. Patients carry or wear the battery pack, which is connected to the LVAD by a driveline.
3. Cannula
To connect the LVAD to the heart and circulatory system, two tubes or cannulas are used. One cannula draws blood from the left ventricle, and the other delivers it to the aorta. These cannulas are crucial for the proper functioning of the LVAD.
4. Controller
The external controller is a fundamental component of the LVAD system. It monitors and controls the LVAD's functions, ensuring that it operates efficiently and maintains optimal blood flow. Healthcare providers can also adjust the device's settings using the controller.
5. Driveline
The driveline is a subcutaneous tube that connects the LVAD's internal pump to the external controller and power source. It allows the passage of power and control signals between the internal and external components of the LVAD.
6. Monitoring and Alarms
Most LVADs are equipped with monitoring systems and alarms that alert the patient and healthcare providers to potential issues. These alarms can indicate low battery, device malfunction, or other critical situations.
Most popular procedures in India
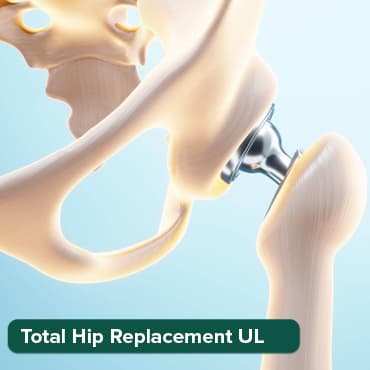
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
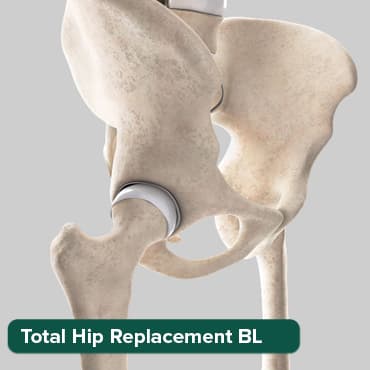
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ANGIOGRAM
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

7. Surgical Components
Various surgical components, such as the anchoring system for the pump, are utilized during the implantation of the LVAD. These components secure the LVAD in the patient's body.
LVAD Surgery: A Lifesaving Procedure
1. Preoperative Evaluation
Before the LVAD surgery, a thorough preoperative evaluation is conducted. This assessment includes cardiac evaluations, laboratory tests, and imaging studies to determine the extent of heart failure and the suitability of the patient for an LVAD.
2. Anesthesia Induction
The patient is taken into the operating room, and general anesthesia is administered to ensure that they are completely unconscious and free from pain during the surgical procedure.
3. Incisions and Access
Multiple incisions are carefully made in the chest and abdomen. These incisions serve as access points for the surgeon to reach the heart, blood vessels, and the implantation site for the LVAD. The specific locations of these incisions may vary based on the patient's anatomy and the chosen LVAD model.
4. Cannula Placement
Two cannulas, or tubes, are inserted into the patient's circulatory system. One cannula is positioned in the left ventricle, while the other is inserted into the aorta. These cannulas are essential for connecting the LVAD, rerouting blood flow, and assisting the heart's pumping function.
5. Implantation of LVAD
The LVAD pump is surgically implanted within the patient's chest. The precise technique for implantation may vary depending on the specific LVAD model. Common locations for the LVAD pump include the abdominal wall or just below the heart.
6. Connection to Controller and Power Source
The LVAD is connected to an external controller and power source. A subcutaneous driveline is passed through the patient's abdominal wall to establish the connection between the internal pump and the external equipment. The controller continuously monitors and regulates the LVAD's operation to maintain optimal blood flow.
7. Testing and Calibration
The surgical team conducts rigorous testing to ensure the LVAD is functioning correctly. The device is calibrated to the patient's specific requirements, and settings are adjusted as needed to optimize blood flow while minimizing complications.
8. Closure of Incisions
The incisions created during the surgery are closed using sutures or staples, and the surgical wound is dressed and bandaged.
9. Postoperative Care
Following the surgery, the patient is closely monitored in the intensive care unit (ICU) or a specialized cardiac care unit. Medications are administered to prevent infections, blood clots, and to support the LVAD's function.
10. Recovery and Rehabilitation
The patient's recovery process varies, but it typically involves a period of rehabilitation and patient education. This includes learning how to care for the LVAD, recognizing potential complications, and adapting to the necessary lifestyle changes, such as dietary restrictions and regular medical follow-up.
Potential Risks of LVAD Therapy
LVAD (Left Ventricular Assist Device) therapy is a life-saving intervention for individuals with severe heart failure. However, like any medical procedure, it carries certain risks and potential complications that patients and healthcare providers must consider. Here are some of the key potential risks associated with LVAD therapy:
1. Infection
Infection is a significant concern for LVAD recipients. The driveline, a tube that connects the LVAD pump to the external controller and power source, creates an entry point for bacteria. Patients must be vigilant about proper driveline care and hygiene to minimize the risk of infection. In some cases, infections can be severe and lead to systemic illness.
2. Bleeding
The use of blood-thinning medications, necessary to prevent clot formation within the LVAD, can increase the risk of bleeding. Patients need to carefully manage their medication and be alert to any signs of bleeding, such as easy bruising, prolonged bleeding from cuts or wounds, or blood in the stool or urine.
3. Stroke
Stroke is another potential risk associated with LVAD therapy. The altered blood flow within the LVAD can sometimes lead to clot formation. These clots can potentially embolize and travel to the brain, causing a stroke. Close monitoring and appropriate medication management are essential to reduce this risk.
4. Device Malfunctions
While LVADs are designed for durability, they are mechanical devices and can experience device malfunctions. These malfunctions may include pump stoppage, driveline issues, or power source problems. Regular device monitoring and prompt action in response to alarms are critical to identifying and addressing malfunctions.
5. Right Heart Failure
The right heart can be affected when an LVAD is implanted. It may have to work harder to pump blood into the lungs, which can lead to right heart failure. Right heart failure can cause symptoms such as swelling in the legs, fluid retention, and shortness of breath.
6. Gastrointestinal Complications
LVAD therapy can sometimes lead to gastrointestinal complications, including gastrointestinal bleeding or conditions like arteriovenous malformations. Patients should be monitored for signs of gastrointestinal distress and receive appropriate care
Benefits of LVADs (Left Ventricular Assist Devices)
1. Improved Quality of Life
LVADs provide individuals with severe heart failure an opportunity to regain an improved quality of life. They can often resume many activities and routines they were unable to perform due to their heart condition.
2. Bridge to Transplant
LVADs serve as a "bridge" for patients awaiting heart transplantation. While they wait for a suitable donor heart, the LVAD supports their heart function and helps them maintain a better quality of life.
3. Extended Life Expectancy
LVADs significantly extend the life expectancy of patients with severe heart failure. This allows individuals to spend more time with their loved ones and experience meaningful life events they may have otherwise missed.
4. Symptom Relief
LVADs alleviate the symptoms of heart failure, such as shortness of breath, fatigue, and fluid retention. This relief improves the patient's overall comfort and well-being.
5. Heart Function Improvement
By assisting the left ventricle in pumping blood, LVADs can help the heart rest and potentially recover some of its lost function over time. This is especially valuable for those with reversible causes of heart failure.
6. Enhanced Mobility
Patients with LVADs can regain mobility and independence, allowing them to engage in daily activities, travel, and enjoy a more active lifestyle.
7. Improved Heart Function Assessment
LVADs provide healthcare professionals with a unique opportunity to continuously monitor the heart's function and response to therapy, allowing for more informed decision-making regarding transplantation.
8. Opportunity for Non-Transplant Candidates
For patients who are not suitable candidates for heart transplantation, LVADs offer a long-term treatment option known as destination therapy. This allows them to manage their heart failure and enjoy a better quality of life for an extended period.
9. Patient Support and Education
LVAD programs often provide comprehensive patient support and education to help individuals and their families adapt to life with an LVAD. This includes guidance on device management, dietary adjustments, and recognition of potential complications.
Cost Considerations for LVADs
The financial aspects of LVAD therapy are a critical factor to consider when evaluating this life-saving treatment. Here are some key points to keep in mind:
1. Average Cost of LVAD Implantation
LVAD implantation is a complex surgical procedure, and the cost can vary significantly depending on various factors. On average, the cost of LVAD implantation is approximately $175,000. However, this figure can be higher or lower depending on the specific circumstances.
2. Ongoing Care Expenses
The costs associated with LVAD therapy extend beyond the initial implantation. Patients must also account for ongoing care and maintenance. The estimated annual expenses for LVAD patients typically range from $30,000 to $50,000. This includes expenses related to medical check-ups, medications, device monitoring, and potential complications.
3. Insurance Coverage
Health insurance plays a pivotal role in managing the financial burden of LVAD therapy. Many insurance plans, including Medicare and Medicaid, provide coverage for LVAD implantation and related medical expenses. It's crucial for patients to thoroughly review their insurance policies to understand what is covered and what out-of-pocket expenses they may incur.
4. Financial Planning
Before embarking on LVAD therapy, it is advisable to engage in financial planning. This may involve assessing personal savings, evaluating insurance coverage, and exploring potential financial assistance programs or grants. Open and transparent discussions with healthcare providers and insurance representatives can help individuals make well-informed decisions about the financial aspects of LVAD therapy.
Medical and Personal Considerations
LVAD therapy is not solely about financial considerations. There are other critical factors that individuals and their healthcare teams should evaluate when contemplating this treatment:
1. Health and Age
The patient's overall health and age are important considerations. LVAD therapy may be suitable for some, but not all, individuals with heart failure. It is typically recommended for those who have severe heart failure that has not responded to other treatments.
2. Heart Failure Severity
The severity of heart failure is a key determinant in the decision to pursue LVAD therapy. Patients with advanced heart failure, who are classified as Stage D, are more likely to be candidates for this intervention.
3. Patient Expectations and Goals
Individual patient expectations and goals of treatment are vital. Open and honest discussions with healthcare providers about the potential benefits and limitations of LVAD therapy are essential to set realistic expectations.
4. Potential Risks
Understanding the potential risks of LVAD therapy is crucial. Patients should be aware of complications such as infection, bleeding, and stroke, and how these may be managed or mitigated.
Additional Considerations
Beyond the financial and medical aspects, individuals and their families should be aware of additional considerations when opting for LVAD therapy:
1. Lifestyle Changes
LVAD recipients may need to adapt their lifestyle to accommodate the device. This can include avoiding strenuous physical activities and adhering to a medication regimen to prevent blood clots.
2. Emotional Impact
LVAD therapy can be emotionally challenging for both patients and their families. Coping with the adjustment to life with an LVAD may require a strong support system and access to mental health resources.
3. Social Impact
Social aspects, such as limiting travel and avoiding crowded places, may also be impacted by LVAD therapy. Discussing these potential changes with loved ones and planning accordingly is essentia
Challenges and Considerations of LVADs (Left Ventricular Assist Devices)
1. Risk of Infection
Patients with LVADs are at an increased risk of developing driveline infections, which are infections occurring at the site where the LVAD's driveline exits the body. Vigilant care and infection prevention measures are crucial.
2. Bleeding and Blood Thinning
LVAD recipients often require blood-thinning medications to prevent clot formation within the device. However, these medications can increase the risk of bleeding complications.
3. Device Malfunctions
Like any mechanical device, LVADs can experience mechanical issues or malfunctions. Regular monitoring and maintenance are essential to ensure the device functions correctly.
4. Lifestyle Adjustments
Patients must adapt to various lifestyle changes when living with an LVAD. This includes dietary restrictions, limitations on certain physical activities, and a commitment to regular medical check-ups.
5. Driveline Management
Managing the driveline that connects the LVAD to the external controller and power source is a critical aspect of LVAD care. Proper care and attention are necessary to prevent complications at this site.
6. Device Dependence
LVAD recipients become dependent on the device for heart function. This dependence can affect daily routines and activities, as well as create anxiety related to device reliability.
7. Ongoing Medical Follow-up
Patients with LVADs require continuous medical monitoring to assess device function, manage complications, and make necessary adjustments to optimize their care.
8. Psychological and Emotional Impact
Living with an LVAD can be emotionally challenging. Patients may experience anxiety, depression, and stress related to their condition and the lifestyle adjustments it necessitates.
9. Financial Considerations
The cost of LVAD implantation, follow-up care, and device maintenance can be substantial. Financial considerations and insurance coverage are essential for patients and their families to plan for.
10. Complications and Emergencies
LVAD recipients need to be educated on recognizing and managing potential complications, such as bleeding, clotting, or device alarms, and be prepared for emergencies.
Future Directions and Advancements in LVAD Technology
1. Miniaturization
Researchers are actively working on making LVADs smaller and more portable. Miniaturized devices may reduce the invasiveness of implantation procedures and improve patient comfort, making LVADs accessible to a broader range of patients.
2. Improved Biocompatibility
Enhancements in materials science are expected to lead to LVADs with improved biocompatibility. This could reduce the risk of blood clots, infections, and other complications associated with the device.
3. Fully Implantable Devices
One of the future goals in LVAD technology is the development of fully implantable devices. These LVADs would eliminate the need for external equipment, further enhancing patient mobility and quality of life.
4. Artificial Intelligence and Remote Monitoring
The integration of artificial intelligence (AI) and remote monitoring systems is on the horizon. This would enable real-time monitoring of LVAD performance, allowing healthcare providers to detect issues early and make timely adjustments or interventions.
5. Destination Therapy Refinements
For patients who are not eligible for heart transplantation, advancements in LVAD technology will focus on making destination therapy even more effective and improving long-term outcomes. This may involve refining the device design and reducing the risk of complications.
6. Cost Reduction
Efforts are ongoing to reduce the overall cost of LVADs and associated care. Reducing costs would expand access to this life-saving technology for a broader population of heart failure patients.
7. Enhanced Energy Sources
Future advancements may bring about more efficient and long-lasting power sources for LVADs. This could reduce the need for frequent battery changes and enhance patient convenience.
8. Enhanced User Interfaces
Improvements in user interfaces for LVADs may make them more user-friendly and allow patients to better manage their devices. This could include smartphone apps and user-friendly displays for monitoring device status and making adjustments.
Real-Life Inspirations: Patient Stories of LVAD Success
One of the most compelling aspects of the LVAD journey is the resilience and determination demonstrated by patients who have benefited from this groundbreaking technology. Their stories are a testament to the hope, strength, and transformation that LVADs bring into their lives. Let's delve into a few remarkable patient stories that showcase the positive impact of LVADs:
1. Sarah's Second Chance at Life
- Sarah, a 48-year-old mother of two, was living with severe heart failure due to a rare genetic condition. Her heart was weak, and simple activities had become a struggle. She faced the daunting prospect of leaving her children without a mother. But everything changed when Sarah became an LVAD recipient. With her LVAD implant, she experienced a remarkable improvement in her quality of life. She could once again play with her kids, go for walks, and even enjoy family outings. Sarah's story is a heartwarming reminder of how LVADs offer a second chance at life and precious moments with loved ones.
2. John's Bridge to a New Heart
- John had been on the heart transplant waiting list for over a year. His heart was failing, and his health was rapidly deteriorating. Then, his healthcare team recommended an LVAD as a bridge to transplant. The LVAD would keep him alive and improve his overall health while he awaited a suitable donor heart. Thanks to the LVAD, John's condition stabilized, and he could participate in cardiac rehabilitation to regain his strength. After a long and anxious wait, John finally received a heart transplant, and he attributes his successful recovery to the LVAD that gave him the gift of time.
3. Mary's Journey with Destination Therapy
- Mary, a 72-year-old retired schoolteacher, was diagnosed with end-stage heart failure. While not a candidate for heart transplantation due to her age, Mary still had a strong desire to enjoy her remaining years to the fullest. She opted for LVAD implantation as a destination therapy. The LVAD significantly improved her heart function, allowing her to continue her hobbies, travel, and spend precious time with her grandchildren. Mary's story underscores the value of LVADs as a destination therapy for those who may not have other treatment options.
4. Sam's Athletic Comeback
- Sam was an avid athlete in his youth, but his dreams of an active life were shattered when he was diagnosed with severe heart failure. After receiving an LVAD, he worked closely with his healthcare team to rebuild his strength. Sam's dedication and the support of his LVAD allowed him to return to his favorite sports, running marathons, and achieving goals he once thought were unattainable. His story exemplifies the determination and resilience LVAD recipients can display when given the opportunity to regain their lives.
5. Grace's Advocacy for LVAD Awareness
- After receiving an LVAD, Grace was inspired to advocate for heart health awareness and LVAD education. She started a support group for LVAD patients and their families, providing a safe space to share experiences and provide emotional support. Grace's commitment to raising awareness and offering support has made a significant impact on the LVAD community. Her story highlights the importance of support networks and community-building for those living with LVADs.
Conclusion
The development and widespread use of LVADs have revolutionized cardiac care, offering a lifeline to individuals with severe heart failure. These mechanical pumps provide hope and a renewed lease on life for those who would otherwise have limited options. As medical technology continues to advance, it is expected that LVADs will become even more efficient, reliable, and accessible, further improving the lives of those with cardiac conditions.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!






