
Liver Transplants and Recovery in the UAE
20 Nov, 2023
 Healthtrip
HealthtripIntroduction
- Liver transplant is a life-saving procedure for individuals suffering from end-stage liver disease. In the United Arab Emirates (UAE), the medical infrastructure is well-equipped to provide advanced healthcare services, including liver transplants. This guide outlines the detailed procedure of liver transplant in the UAE.
1. Preliminary Assessments
1.1. Patient Evaluation
Before undergoing a liver transplant, a thorough assessment of the patient's medical history, current health status, and liver function is conducted. This involves blood tests, imaging studies, and consultations with specialists to determine the necessity and feasibility of the transplant.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

1.2. Compatibility Tests
Identification of a suitable donor is crucial. Family members are often the first choice, but in cases where a living donor is not available, deceased donor transplants are considered. Compatibility tests ensure a match and reduce the risk of rejection.
2. Candidacy and Evaluation
2.1. Multidisciplinary Evaluation
A team of healthcare professionals, including hepatologists, transplant surgeons, psychologists, and nutritionists, collaborates to evaluate the patient's overall health. This multidisciplinary approach ensures a comprehensive understanding of the patient's condition.
2.2. Psychological Assessment
Patients must undergo psychological evaluations to assess their mental and emotional readiness for the transplant process. This is essential for post-transplant coping and adherence to the prescribed medication regimen.
3. Registration and Waiting List
3.1. United Network for Organ Sharing (UNOS) Registration
Patients in need of a liver transplant are registered with UNOS, a network that facilitates organ allocation. The waiting time varies depending on factors such as blood type, severity of the condition, and donor availability.
3.2. Priority Criteria
Patients are prioritized based on the severity of their liver disease, medical urgency, and time spent on the waiting list. This ensures that the organs are allocated to those who need them the most.
4. Transplant Surgery
4.1. Preoperative Preparation
Once a suitable donor is identified, both the recipient and the donor undergo preoperative preparations. The recipient is prepared for surgery, while the donor undergoes a comprehensive health check.
Most popular procedures in
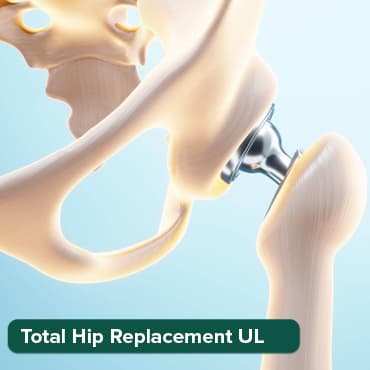
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
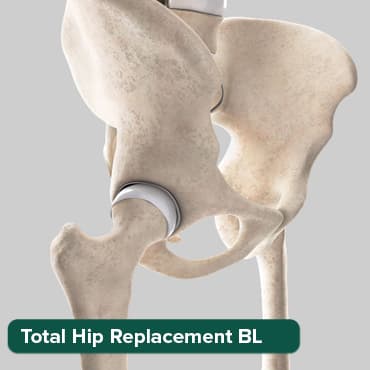
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Breast Cancer Surger
Upto 80% off
90% Rated
Satisfactory

Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory
Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory

4.2. Liver Transplant Procedure
The transplant surgery involves removing the diseased liver and replacing it with the healthy donor liver. The surgical team carefully connects blood vessels and bile ducts to ensure proper functioning of the new liver.
5. Postoperative Care
5.1. Intensive Care Unit (ICU) Stay
After the surgery, the patient is closely monitored in the ICU to manage any immediate postoperative complications. This phase is critical for the early detection and treatment of potential issues.
5.2. Immunosuppression Medications
To prevent organ rejection, patients are prescribed immunosuppressive medications. Strict adherence to this medication regimen is crucial for the long-term success of the transplant.
6. Follow-Up Care
6.1. Outpatient Visits
Regular follow-up visits with the transplant team are essential to monitor the patient's progress, adjust medications, and address any emerging issues. These visits help ensure the ongoing health of the transplanted liver.
6.2. Lifestyle Modifications
Patients are advised to make lifestyle modifications, including a healthy diet, regular exercise, and avoiding alcohol and certain medications that may harm the transplanted liver.
What to Expect During and After Liver Transplant in the UAE?
During the Transplant Procedure
1. Anesthesia and Incision
- Anesthesia: Before the surgery, you will be administered general anesthesia to ensure you are unconscious and pain-free during the procedure.
- Incision: The surgeon makes an incision in the upper abdomen to access the liver. The size and location of the incision may vary.
2. Liver Removal and Transplant
- Diseased Liver Removal: The surgeon removes the diseased liver, disconnecting blood vessels and bile ducts.
- Donor Liver Implantation: The healthy donor liver is then carefully connected to blood vessels and bile ducts.
3. Duration of Surgery
- Varied Duration: The duration of the transplant surgery can vary but typically ranges from 6 to 12 hours. The surgical team ensures precision and thoroughness.
After the Transplant Procedure
1. Initial Recovery in ICU
- Close Monitoring: After the surgery, you will be transferred to the Intensive Care Unit (ICU) for close monitoring of vital signs and immediate postoperative care.
- Ventilator Support: In some cases, ventilator support may be provided initially to assist with breathing.
2. Postoperative Pain Management
- Pain Control: Pain management is a priority, and medications will be administered to control pain and ensure your comfort.
- Transition to Oral Medications: As recovery progresses, pain medications may transition from intravenous to oral forms.
3. Immunosuppression Medications
- Early Initiation: Immediately after the transplant, you will be started on immunosuppressive medications to prevent organ rejection.
- Monitoring Levels: Blood tests will be conducted regularly to monitor the levels of these medications and adjust dosages as needed.
4. Monitoring for Complications
- Vital Sign Monitoring: Continuous monitoring of vital signs, including heart rate, blood pressure, and oxygen levels, is standard practice.
- Complication Surveillance: Healthcare providers closely watch for potential complications, such as infection or issues with the transplanted liver.
5. Transition to Regular Room
- Stable Condition: Once your condition stabilizes, you will be transferred from the ICU to a regular hospital room.
- Continued Monitoring: Monitoring continues, and the healthcare team will assess your overall recovery progress.
6. Rehabilitation and Physiotherapy
- Early Mobilization: Physiotherapy begins early to encourage mobility and prevent complications like blood clots.
- Rehabilitation Program: A structured rehabilitation program is initiated to aid recovery and regain strength.
7. Follow-Up Visits and Outpatient Care
- Postoperative Care Plan: A comprehensive postoperative care plan is established, including regular follow-up visits with the transplant team.
- Monitoring Long-Term Health: Ongoing monitoring ensures the long-term health of the transplanted liver, and adjustments to medications are made as necessary.
8. Psychological Support and Counseling
- Emotional Well-being: Emotional well-being is addressed through counseling and support groups to help cope with the psychological aspects of the transplant journey.
- Family Involvement: Involving family members in the recovery process is encouraged for additional support.
Post-Transplant Period and Long-Term Expectations
9. Discharge and Home Recovery
9.1. Discharge Process
- Stable Condition: Upon reaching a stable condition, you will be discharged from the hospital.
- Home Recovery Plan: The healthcare team will provide detailed instructions for home recovery, including medications, dietary guidelines, and signs to watch for any complications.
9.2. Home Care Assistance
- Home Nurse Support: In some cases, a home nurse may be arranged to assist with medication administration and monitor your recovery.
- Telehealth Follow-Ups: Virtual follow-up appointments may be scheduled to assess your progress and address any concerns.
10. Managing Medications and Follow-Up Appointments
10.1. Medication Adherence
- Crucial Importance: Strict adherence to immunosuppressive medications is crucial to prevent organ rejection.
- Regular Blood Tests: Regular blood tests will be conducted to monitor medication levels and liver function.
10.2. Follow-Up Appointments
- Scheduled Visits: Follow-up appointments with the transplant team will be scheduled at regular intervals.
- Monitoring and Adjustments: During these visits, the team will monitor your overall health, adjust medications if necessary, and address any emerging issues.
11. Resuming Normal Activities
11.1. Gradual Resumption
- Physical Activity: Gradually resume physical activities under the guidance of the healthcare team and physiotherapists.
- Returning to Work: The timing for returning to work will depend on individual recovery progress and the nature of the job.
11.2. Dietary Considerations
- Nutritional Guidance: Follow dietary guidelines provided by nutritionists to support overall health.
- Gradual Diet Transition: Transition from a liquid to a solid diet is typically a gradual process.
12. Potential Challenges and Complications
12.1. Rejection and Infections
- Vigilant Monitoring: Vigilant monitoring for signs of rejection or infections is ongoing.
- Prompt Intervention: Early detection allows for prompt intervention and minimizes potential complications.
12.2. Long-Term Medication Side Effects
- Management Strategies: The healthcare team will work with you to manage any long-term side effects of immunosuppressive medications.
- Balancing Act: Balancing the need for immunosuppression with minimizing side effects is an ongoing process.
13. Quality of Life Improvements
13.1. Restoration of Health
- Renewed Energy: Many recipients experience a significant improvement in energy levels and overall health.
- Resolution of Symptoms: Symptoms related to liver disease often resolve post-transplant.
13.2. Emotional Well-being
- Psychosocial Benefits: Enhanced emotional well-being and improved quality of life are common post-transplant outcomes.
- Support Network: Continued involvement in support groups or counseling contributes to a positive mental outlook.
Conclusion
Undergoing a liver transplant in the UAE is a complex yet well-orchestrated process. From initial evaluations to long-term follow-up care, the commitment of healthcare professionals in the UAE ensures the best possible outcomes for patients. As technology and medical knowledge continue to evolve, the landscape of liver transplantation will undoubtedly see further improvements, offering hope to those in need of this life-saving procedure.
Always consult with medical professionals for the most accurate and up-to-date information regarding liver transplant procedures in the UAE. Each patient's journey is unique, and personalized care is essential for a successful outcome. Facing liver disease with a transplant is a challenging but transformative experience, and the support of healthcare teams, loved ones, and the broader community is instrumental in this journey towards renewed health and vitality
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!






