
Diabetes and Hyperlipidemia: A Dual Diagnosis
21 Oct, 2023
 Healthtrip
HealthtripIntroduction
Diabetes and hyperlipidemia are two common medical conditions that often coexist, leading to a dual diagnosis that can have significant implications for an individual's health. While both conditions are distinct, they frequently intersect, making it crucial to understand their relationship, causes, and management. In this blog, we will explore diabetes and hyperlipidemia as a dual diagnosis, often referred to as "diabetic dyslipidemia." We will delve into the H2 aspect - the hypothesis, the harmony, and the healthcare measures taken to address this dual diagnosis effectively.
1. Hypothesis: Understanding the Relationship
To delve deeper into the dual diagnosis of diabetes and hyperlipidemia, it is crucial to establish a clear understanding of theunderlying hypothesis. This hypothesis forms the cornerstone of the complex relationship between these two conditions and provides valuable insights into how they intersect and influence one another. Let's explore this hypothesis in detail:
1.1. Insulin Resistance: The Common Link
One of the central pillars of the hypothesis is insulin resistance. In diabetes, particularly type 2 diabetes, the body's cells become resistant to the effects of insulin, a hormone responsible for regulating blood sugar levels. Insulin resistance results in elevated blood glucose levels, a hallmark of diabetes.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

1.2. A Cascade of Metabolic Abnormalities
Insulin resistance sets in motion a cascade of metabolic abnormalities. When the cells don't respond effectively to insulin, the body compensates by producing more insulin. This surge in insulin levels has a profound impact on lipid metabolism, giving rise to diabetic dyslipidemia.
1.3. Dysregulated Lipid Metabolism
Diabetic dyslipidemia is characterized by several key features, including:
1. Elevated Triglycerides
- Increased production of triglycerides due to insulin resistance.
- Reduced clearance of triglyceride-rich lipoproteins.
2. Low HDL Cholesterol
- Decreased levels of high-density lipoprotein (HDL) cholesterol, the "good" cholesterol.
- HDL cholesterol plays a vital role in reducing cardiovascular risk.
3. Small, Dense LDL Particles
- Increased prevalence of small, dense low-density lipoprotein (LDL) particles.
- These small particles are more atherogenic, contributing to the development of atherosclerosis.
4. Elevated Total Cholesterol
- Elevated total cholesterol levels are often observed in individuals with diabetes, further increasing their cardiovascular risk.
2. Interplay and Cardiovascular Implications
Understanding the hypothesis helps us recognize how diabetes and hyperlipidemia intersect to create a high-risk scenario for cardiovascular disease:
- Atherosclerosis: Diabetes accelerates the formation of atherosclerotic plaques within arteries, which is further compounded by the lipid imbalances seen in hyperlipidemia. This combination increases the risk of arterial blockages, atherosclerosis, and its associated complications.
- Endothelial Dysfunction: Both conditions, individually and synergistically, lead to endothelial dysfunction. This is a key step in the development of atherosclerosis as it impairs the inner lining of blood vessels, promoting the initiation and progression of plaque formation.
- Inflammation: Chronic inflammation is a common feature of both diabetes and hyperlipidemia. Inflammation within the blood vessels promotes plaque instability, making the arterial walls more prone to rupture, leading to acute cardiovascular events like heart attacks and strokes.
- Oxidative Stress: Elevated levels of reactive oxygen species and oxidative stress in diabetes and hyperlipidemia further contribute to cardiovascular damage. Oxidative stress can exacerbate inflammation and contribute to the deterioration of arterial health.
2. Key Features of Diabetic Dyslipidemia
To gain a deeper understanding of diabetic dyslipidemia, it's crucial to explore the key features that define this condition. These distinctive characteristics shed light on how lipid metabolism is altered in individuals with diabetes. Here are the primary key features of diabetic dyslipidemia:
1. Elevated Triglycerides
Elevated triglyceride levels are a hallmark of diabetic dyslipidemia. This occurs due to a combination of factors, including increased production of triglycerides by the liver and decreased clearance of triglyceride-rich lipoproteins from the bloodstream. Elevated triglycerides are a significant contributor to the increased cardiovascular risk associated with diabetes.
2. Low HDL Cholesterol
Individuals with diabetes often exhibit reduced levels of high-density lipoprotein (HDL) cholesterol, commonly known as "good" cholesterol. HDL cholesterol plays a pivotal role in protecting against cardiovascular disease by facilitating the removal of excess cholesterol from the bloodstream. Low HDL levels further amplify the risk of atherosclerosis and heart disease.
Most popular procedures in
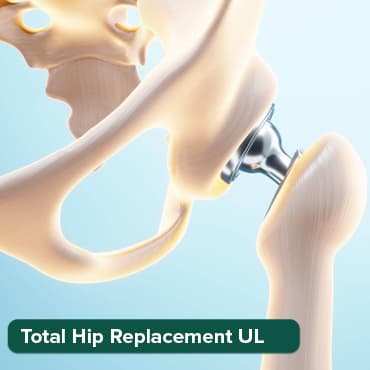
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Breast Cancer Surger
Upto 80% off
90% Rated
Satisfactory

Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory
Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory

3. Small, Dense LDL Particles
Diabetic dyslipidemia is characterized by an increased number of small, dense low-density lipoprotein (LDL) particles. These smaller LDL particles are more atherogenic (likely to contribute to atherosclerosis) than larger, buoyant LDL particles. They have a higher propensity to penetrate arterial walls, promoting the development of arterial plaque and increasing the risk of cardiovascular events.
4. Elevated Total Cholesterol
In individuals with diabetes, total cholesterol levels may also be elevated. Elevated total cholesterol, when combined with other lipid abnormalities, significantly contributes to the overall cardiovascular risk. It is essential to address and manage these elevated cholesterol levels to reduce the risk of heart disease and stroke.
3. Harmony: Impact on Cardiovascular Health
The dual diagnosis of diabetes and hyperlipidemia, known as diabetic dyslipidemia, establishes a profound connection between these two conditions and their combined effect on cardiovascular health. This section delves into the harmony of diabetes and hyperlipidemia, shedding light on the critical impact on cardiovascular well-being.
3.1. Atherosclerosis: A Joint Accelerator
One of the key areas of harmony between diabetes and hyperlipidemia is the accelerated development of atherosclerosis, a condition characterized by the accumulation of plaque within arteries. This phenomenon is of paramount significance for cardiovascular health:
- Diabetes Contribution: Diabetes fosters a pro-inflammatory and pro-thrombotic environment. Insulin resistance and hyperglycemia promote the formation of atherosclerotic plaques.
- Hyperlipidemia Contribution: Hyperlipidemia, particularly the presence of elevated LDL cholesterol levels, contributes to the buildup of cholesterol-rich deposits within the arterial walls, further enhancing the progression of atherosclerosis.
3.2. Endothelial Dysfunction: A Common Consequence
Both diabetes and hyperlipidemia independently and synergistically contribute to endothelial dysfunction. The endothelium, the inner lining of blood vessels, plays a crucial role in maintaining vascular health:
- Diabetes Impact: Chronic high blood glucose levels in diabetes can cause oxidative stress, inflammation, and damage to the endothelial lining, impairing its ability to regulate vascular tone and prevent clot formation.
- Hyperlipidemia Impact: The presence of excess lipids, particularly oxidized LDL cholesterol, within the blood vessels triggers inflammation and further damages the endothelium. This dysfunction creates an environment conducive to plaque formation.
3.3. Inflammation: A Shared Risk Factor
Chronic inflammation is a common thread that links both diabetes and hyperlipidemia. Inflammation is a pivotal player in cardiovascular disease:
- Diabetes and Inflammation: Diabetes is associated with systemic inflammation, characterized by elevated levels of inflammatory markers. This inflammatory state contributes to atherosclerosis progression and cardiovascular complications.
- Hyperlipidemia and Inflammation: Hyperlipidemia, especially the presence of high levels of LDL cholesterol, can initiate and propagate inflammation within the arterial walls. This chronic inflammation accelerates plaque instability.
3.4. Oxidative Stress: A Culprit in Cardiovascular Damage
The dual diagnosis of diabetes and hyperlipidemia also shares a common feature in the form of oxidative stress:
- Diabetes and Oxidative Stress: Hyperglycemia and insulin resistance in diabetes generate reactive oxygen species, leading to oxidative stress. This oxidative stress exacerbates the inflammatory environment within blood vessels, contributing to cardiovascular damage.
- Hyperlipidemia and Oxidative Stress: The presence of excess lipids, particularly oxidized LDL cholesterol, amplifies oxidative stress. The interplay between hyperlipidemia and oxidative stress further deteriorates arterial health.
4. Healthcare Measures: Addressing the Dual Diagnosis
The dual diagnosis of diabetes and hyperlipidemia necessitates a multifaceted approach that combines lifestyle modifications, pharmacological interventions, and regular monitoring to effectively manage both conditions and reduce the associated cardiovascular risk. This section explores the critical healthcare measures that are essential for addressing this dual diagnosis.
1. Lifestyle Modification
Lifestyle modification plays a pivotal role in managing the dual diagnosis of diabetes and hyperlipidemia. It involves adopting and sustaining healthier habits that positively impact both conditions:
- Dietary Changes: Encourage individuals to follow a balanced diet, rich in fruits, vegetables, whole grains, and lean proteins. Limiting saturated fats, trans fats, and refined sugars is crucial. Dietary modifications should aim to improve glycemic control and optimize lipid profiles.
- Regular Physical Activity: Promote regular physical exercise tailored to an individual's fitness level and preferences. Exercise helps with weight management, improving insulin sensitivity, and enhancing overall cardiovascular health.
- Weight Management: Weight control is particularly important in the management of these conditions, as excess body weight can exacerbate insulin resistance and dyslipidemia.
2. Pharmacological Interventions
In many cases, lifestyle modifications may not be sufficient to adequately manage diabetes and hyperlipidemia. Healthcare providers may prescribe medications to address specific aspects of these conditions:
- Statins: These medications are commonly prescribed to manage hyperlipidemia by reducing LDL cholesterol levels and decreasing the risk of cardiovascular events.
- Fibrates: Fibrates are another class of drugs that can help lower triglyceride levels and increase HDL cholesterol, addressing the lipid abnormalities in diabetic dyslipidemia.
- Cholesterol-Absorption Inhibitors: Medications like ezetimibe can be prescribed to reduce the absorption of cholesterol from the diet and lower LDL cholesterol levels.
3. Antidiabetic Medications
The choice of antidiabetic medications should consider their impact on lipid profiles:
- Metformin: This common antidiabetic medication has the added benefit of improving insulin sensitivity and may have a positive effect on lipid profiles.
- GLP-1 Receptor Agonists: Some GLP-1 receptor agonists have been shown to reduce cardiovascular risk and improve glycemic control in individuals with diabetes.
- SGLT-2 Inhibitors: Certain SGLT-2 inhibitors have demonstrated cardiovascular benefits and may be considered for individuals with both diabetes and hyperlipidemia.
4. Regular Monitoring
Frequent monitoring of blood glucose levels, lipid panels, and cardiovascular risk factors is essential:
- Blood Glucose Monitoring: Regular self-monitoring of blood glucose levels is vital for individuals with diabetes to ensure glycemic control.
- Lipid Profiles: Regular lipid panels help track cholesterol levels, including LDL, HDL, and triglycerides.
- Blood Pressure Monitoring: High blood pressure often coexists with diabetes and hyperlipidemia, making regular blood pressure checks crucial.
5. Individualized Care
Recognize that the dual diagnosis varies among individuals. Tailoring treatment plans to address the unique needs, preferences, and responses of each patient is essential for effective management.
6. Patient Education
Educate patients about the importance of adhering to their treatment plans, making necessary lifestyle changes, and consistently taking prescribed medications. Empower them with knowledge about their conditions and how to manage them effectively.
5. Prevention and Early Intervention: A Vital Aspect
Preventing the onset of diabetes and hyperlipidemia, or intervening early in the disease process, is a critical component of healthcare. By addressing risk factors and taking proactive measures, healthcare providers can reduce the incidence and severity of these conditions, ultimately leading to improved public health. Here are key aspects of prevention and early intervention:
1. Primary Prevention
Primary prevention strategies aim to reduce the initial occurrence of diabetes and hyperlipidemia. These approaches are essential in addressing the root causes of these conditions and include:
- Promoting Healthy Lifestyles: Encourage individuals to adopt healthy lifestyles early in life. Emphasize the importance of a balanced diet, regular physical activity, and weight management. Prevention efforts should begin in childhood and continue throughout life.
- Educating the Public: Raise public awareness about the risks associated with diabetes and hyperlipidemia. Inform people about modifiable risk factors, such as diet and physical inactivity, and the importance of early intervention.
- Community Programs: Develop and support community programs that focus on nutrition education, physical activity, and obesity prevention.
2. Screening and Early Detection
Early detection of diabetes and hyperlipidemia is crucial to prevent the progression of these conditions. Healthcare providers should:
- Include Routine Screenings: Regular medical check-ups should include screenings for both diabetes and hyperlipidemia, particularly for individuals with risk factors such as family history, obesity, or a sedentary lifestyle.
- Assess Risk Factors: Evaluate patients' risk factors, including age, family history, and lifestyle habits. This information can guide the frequency and timing of screenings.
- Leverage Technology: Utilize modern diagnostic tools and technologies to facilitate early detection, including blood tests and imaging methods to assess lipid profiles and glucose metabolism.
3. Education and Awareness
Educating the public about the risks and potential consequences of diabetes and hyperlipidemia is fundamental. This education can empower individuals to make informed decisions and take steps to mitigate risk:
- Public Campaigns: Engage in public health campaigns to raise awareness about the link between lifestyle choices, diabetes, and hyperlipidemia. These campaigns can disseminate information on healthy living and the importance of regular check-ups.
- School-Based Education: Incorporate health education programs into school curricula to teach children and young adults about the significance of a healthy lifestyle and early disease prevention.
- Patient Education: Healthcare providers should educate their patients about the risk factors, warning signs, and the benefits of early intervention. Providing resources and guidance on lifestyle changes is crucial.
6. Holistic Patient-Centered Care
The management of the dual diagnosis of diabetes and hyperlipidemia necessitates a patient-centered approach that encompasses the broader well-being of individuals. Holistic patient-centered care is vital in recognizing the unique needs and challenges of each patient and tailoring treatment plans to address the physical, psychological, and social aspects of their health.
1. Shared Decision-Making
Collaboration between healthcare providers and patients is at the core of patient-centered care. This approach involves open and empathetic communication, allowing patients to actively participate in decisions about their treatment, lifestyle modifications, and medication choices. Shared decision-making respects individual preferences and values, leading to more effective and patient-satisfactory outcomes.
2. Psychosocial Support
The psychological and emotional impact of living with both diabetes and hyperlipidemia should not be underestimated. Holistic patient-centered care recognizes the importance of addressing the emotional aspects of these chronic conditions. Healthcare providers should:
- Assess Mental Health: Screen for and address issues such as anxiety, depression, and diabetes-related distress in patients.
- Provide Counseling: Offer counseling and support services to help patients cope with the challenges and emotional aspects of their conditions.
- Address Quality of Life: Recognize that quality of life is a critical outcome. Addressing psychological well-being contributes to a higher overall quality of life.
3. Monitoring and Follow-Up
Regular follow-up appointments are essential in holistic care. These visits serve several purposes:
- Progress Tracking: Continuously monitor the progress of patients, including their glycemic control, lipid profiles, and overall health status.
- Treatment Adjustment: Adjust treatment plans and medications as necessary to ensure optimal management.
- Patient Feedback: Provide an opportunity for patients to voice their concerns, ask questions, and provide feedback on their care.
4. Nutritional Guidance
Diet plays a central role in managing both diabetes and hyperlipidemia. Collaborate with registered dietitians to provide patients with personalized dietary plans. Nutritional guidance aims to:
- Optimize Glycemic Control: Help patients make dietary choices that stabilize blood sugar levels.
- Improve Lipid Profiles: Modify diets to reduce triglycerides, lower LDL cholesterol, and increase HDL cholesterol.
- Promote Balanced Eating: Encourage balanced and sustainable eating habits.
5. Exercise Programs
Regular physical activity is integral to managing diabetes and hyperlipidemia. However, exercise recommendations should be individualized to accommodate patients' fitness levels, preferences, and physical limitations. Exercise programs focus on:
- Improving Insulin Sensitivity: Physical activity helps enhance insulin sensitivity, contributing to better glycemic control.
- Weight Management: Exercise supports weight loss and maintenance, which is particularly beneficial for individuals with both conditions.
- Cardiovascular Health: Regular exercise also benefits heart health, reducing the risk of cardiovascular complications.
7. Research and Innovation
Research and innovation are instrumental in advancing our understanding of diabetes and hyperlipidemia as a dual diagnosis and developing new, more effective treatments. The healthcare field is continuously evolving, and investments in research are key to improving prevention, diagnosis, and management of these conditions. Here's how research and innovation play a pivotal role:
1. Advancing Understanding
Ongoing research endeavors aim to deepen our comprehension of the underlying mechanisms and interplay between diabetes and hyperlipidemia. By unraveling the intricacies of these conditions, researchers can identify novel therapeutic targets and better strategies for management.
- Genetic Studies: Genetic research provides insights into the hereditary components of these conditions, enabling a better understanding of who is at higher risk and why.
- Metabolic Profiling: Cutting-edge techniques like metabolomics allow researchers to profile the metabolic alterations associated with diabetes and hyperlipidemia, paving the way for tailored treatments.
2. Prevention and Early Detection
Research fosters the development of new tools and strategies for preventing diabetes and hyperlipidemia or detecting them at the earliest stages. Early intervention can significantly impact the course of these diseases.
- Biomarkers and Screening: Research is uncovering novel biomarkers that may assist in the early detection of both conditions, enabling prompt intervention.
- Risk Prediction Models: Advanced statistical models are being developed to predict an individual's risk of developing diabetes and hyperlipidemia, facilitating personalized prevention strategies.
3. Innovative Treatment Options
Investments in research lead to the discovery and development of new treatment modalities for diabetes and hyperlipidemia. These innovations can enhance patient outcomes and quality of life.
- Precision Medicine: The emergence of precision medicine allows for tailored treatment approaches based on an individual's genetic, metabolic, and clinical characteristics.
- Novel Medications: Ongoing research results in the development of novel medications that target specific pathways in diabetes and hyperlipidemia, improving efficacy and safety.
- Medical Devices: Innovations in medical devices, such as continuous glucose monitoring systems and non-invasive lipid measurement tools, enhance disease management.
4. Digital Health and Telemedicine
Technological advancements in the form of digital health and telemedicine are transforming the way healthcare is delivered. These innovations provide improved access to care and tools for remote monitoring, helping individuals manage their conditions effectively.
- Telehealth Platforms: Telemedicine allows patients to consult with healthcare providers remotely, facilitating regular check-ups and monitoring of diabetes and hyperlipidemia.
- Mobile Apps: Mobile applications offer tools for tracking blood glucose levels, diet, exercise, and medication adherence, empowering patients to take charge of their health.
5. Collaboration and Interdisciplinary Research
Collaboration between healthcare providers, researchers, and pharmaceutical companies is paramount in advancing our understanding of these conditions and improving treatment options. Interdisciplinary research teams bring together experts from various fields to tackle complex challenges.
- Clinical Trials: Participation in clinical trials is vital to test the safety and efficacy of new treatments, medications, and interventions.
- Data Sharing: Sharing clinical and research data among institutions and researchers accelerates progress and helps identify patterns and insights that can inform better care.
Conclusion
The dual diagnosis of diabetes and hyperlipidemia, or diabetic dyslipidemia, is a complex medical condition with significant implications for cardiovascular health. Understanding the hypothesis, recognizing the harmony between these conditions, and implementing comprehensive healthcare measures are essential steps in managing this dual diagnosis effectively. By addressing both diabetes and hyperlipidemia in a holistic manner, healthcare professionals can reduce the risk of cardiovascular complications and improve the overall well-being of their patients.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!