
Cranioplasty: Understanding the procedure, risks, and outcomes
18 Aug, 2023
 Healthtrip Team
Healthtrip TeamWhat is cranioplasty?
Cranioplasty is a surgical procedure that involves the repair or reconstruction of defects or deformities in the cranial bones. These defects can arise due to various reasons, including trauma, surgical procedures, or congenital conditions. The primary goal of cranioplasty is to restore the integrity of the skull, providing protection to the underlying brain tissue and improving the cosmetic appearance of the head.
The practice of cranioplasty dates back thousands of years, with evidence of trepanation (the act of making a hole in the skull) found in ancient human remains. These early procedures, often performed for ritualistic or therapeutic reasons, are considered the precursors to modern cranioplasty. Ancient civilizations, from the Incas to the Egyptians, have shown evidence of understanding the importance of the skull's integrity and have attempted repairs using various materials, including gold, silver, and even shells. Over the centuries, as medical knowledge and surgical techniques advanced, cranioplasty evolved into the sophisticated procedure we recognize today.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Cranioplasty is not just a cosmetic procedure; it serves several critical functions:
- Protection: The primary role of the skull is to safeguard the delicate brain tissue from external threats. A defect or gap in the skull leaves the brain vulnerable to injuries, infections, and other complications.
- Functional Recovery: For patients who have undergone surgeries like decompressive craniectomy (where a part of the skull is removed to relieve pressure on the brain), restoring the skull's structure can aid in neurological recovery and improve overall brain function.
- Cosmetic Restoration: A defect in the skull can lead to visible deformities, affecting an individual's self-esteem and social interactions. Cranioplasty helps in restoring the natural shape of the head, boosting the patient's confidence.
- Cerebral Hemodynamics: Some studies suggest that cranioplasty can improve cerebral blood flow, which might have positive implications for brain function.
In conclusion, cranioplasty is a vital surgical intervention that goes beyond aesthetics, playing a crucial role in patient recovery, protection, and overall well-being.
Indications for Cranioplasty
Post-traumatic Defects: Traumatic events, such as vehicular accidents, falls, or acts of violence, can lead to fractures or defects in the skull. These defects might not always be immediately apparent, especially if they are covered by scalp tissue. Over time, however, they can pose risks to the underlying brain due to the lack of protection. Cranioplasty in such cases is essential to restore the skull's integrity, ensuring that the brain remains shielded from external threats.
Surgical Defects: Neurosurgical interventions, especially those involving the removal of brain tumors, cysts, or other pathological masses, often require the removal of a portion of the skull to access the affected area. Similarly, procedures like decompressive craniectomy, performed to alleviate increased intracranial pressure, result in intentional defects in the skull. Once the primary medical concern has been addressed, and the patient is stable, cranioplasty is performed to replace the missing or removed bone segment, ensuring both protection and a return to the skull's natural contour.
Congenital Skull Deformities: Some individuals are born with abnormalities in the structure or shape of their skulls. These congenital deformities can range from minor cosmetic issues to significant defects that expose the brain or interfere with its function. In such cases, cranioplasty is indicated not just for aesthetic reasons but also to ensure that the brain develops and functions in an optimal environment.
Cosmetic Reasons: While the primary indications for cranioplasty are often medical in nature, there are instances where individuals seek the procedure purely for cosmetic reasons. This can include correcting minor deformities that might not pose a direct threat to brain function but affect the individual's appearance and self-esteem. With advancements in surgical techniques and materials, cranioplasty can achieve impressive cosmetic results, ensuring that the skull's shape and contour closely match its natural state.
Most popular procedures in
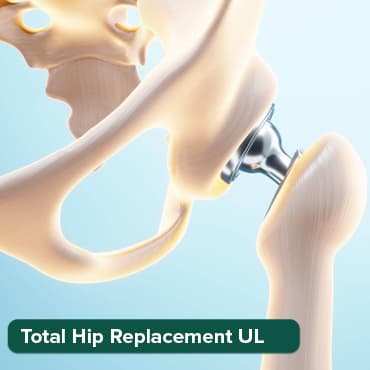
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
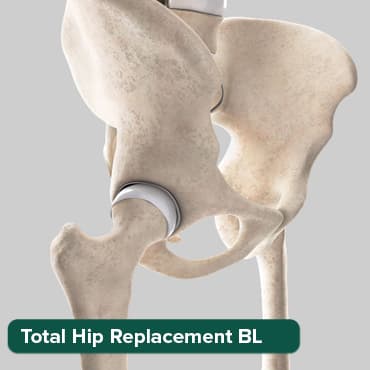
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Breast Cancer Surger
Upto 80% off
90% Rated
Satisfactory

Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory
Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory

In essence, the indications for cranioplasty span a broad spectrum, from addressing life-threatening conditions to enhancing one's appearance. Regardless of the reason, the procedure plays a pivotal role in improving the quality of life for many individuals.
Pre-operative Evaluation for Cranioplasty
Patient History: A comprehensive patient history is the cornerstone of any surgical evaluation. For cranioplasty candidates, understanding the cause of the skull defect is paramount. This involves gathering information about:
- Previous traumatic events or injuries.
- Past surgical interventions, especially neurosurgical procedures.
- Any congenital conditions or hereditary factors that might have contributed to the defect.
- Symptoms experienced by the patient, such as headaches, seizures, or neurological deficits.
- Other relevant medical conditions and medications currently being taken.
Physical Examination: A thorough physical examination focuses on:
- Assessing the size of the defect: This helps in determining the amount of material or graft required.
- Location of the defect: Its position can influence the surgical approach and potential complications.
- Nature of the defect: Whether it's a clean, well-defined gap or a more irregular, fragmented defect.
- Condition of the surrounding scalp tissue: Checking for signs of infection, scarring, or compromised blood supply.
Imaging Studies: Modern imaging techniques provide detailed insights into the structure and condition of the skull:
- CT Scans (Computed Tomography): These offer a clear, cross-sectional view of the skull, highlighting the extent and depth of the defect. Bone windows in CT scans are particularly useful for visualizing bony defects.
- MRI (Magnetic Resonance Imaging): While CT scans are superior for visualizing bone, MRIs provide detailed images of soft tissues, including the brain. This can be crucial if the defect has associated brain injuries or pathologies.
- X-rays: While not as detailed as CT scans or MRIs, X-rays can still offer a quick overview of the skull's structure and the location of the defect.
Neurological Assessment: Before undergoing cranioplasty, a patient's neurological status must be thoroughly evaluated:
- Cognitive function: Assessing memory, attention, and other higher-order functions.
- Motor and sensory examination: Checking for any deficits or abnormalities in movement or sensation.
- Reflexes: Both superficial and deep tendon reflexes are evaluated.
- Special tests, if required, such as electroencephalograms (EEG) to monitor brain electrical activity, especially if the patient has a history of seizures.
The pre-operative evaluation is a meticulous process that ensures the patient is a suitable candidate for cranioplasty and helps the surgical team plan the procedure effectively. Proper assessment minimizes potential complications and maximizes the chances of a successful outcome.
Materials Used in Cranioplasty
1. Autologous Grafts: These are bone grafts harvested from the patient's own body.
- Advantages:
- Biocompatibility: Since the graft is from the patient's own body, there's a reduced risk of rejection or allergic reactions.
- No Risk of Disease Transmission: There's no chance of transmitting infections or diseases from a donor.
- Natural Integration: The bone graft tends to integrate well with the surrounding bone, leading to a more natural and durable repair.
- Disadvantages:
- Additional Surgical Site: Harvesting the bone requires an additional surgical site, which means more potential for complications, pain, and longer recovery.
- Limited Availability: There's a finite amount of bone that can be harvested, especially if the defect is large.
2. Allografts: These are bone grafts sourced from another individual, often from cadaveric donors.
- Advantages:
- No Need for Harvesting: This eliminates the complications and pain associated with an additional surgical site.
- Availability: Suitable for larger defects where autologous bone might be insufficient.
- Disadvantages:
- Risk of Disease Transmission: Even though rigorous screening processes are in place, there's a small risk of transmitting diseases.
- Potential for Rejection: The body might recognize the graft as foreign and mount an immune response against it.
- Lesser Integration: Allografts might not integrate as seamlessly as autologous grafts.
3. Synthetic Materials: These are man-made materials designed for medical applications.
- Titanium Plates:
- Advantages: Strong, durable, and biocompatible. They can be molded to fit the defect precisely.
- Disadvantages: Metallic implants can interfere with some imaging studies like MRI.
- Acrylic (Polymethyl Methacrylate or PMMA):
- Advantages: Easily moldable during surgery, allowing for a custom fit. It's also radiolucent, meaning it doesn't interfere with imaging studies.
- Disadvantages: Not as strong as bone or titanium. There's a potential for infection or extrusion.
- Hydroxyapatite:
- Advantages: Biocompatible and can integrate well with surrounding bone. It's also osteoconductive, meaning it can support bone growth.
- Disadvantages: More brittle than natural bone or titanium, so it might not be suitable for all locations or defect sizes.
When selecting a material for cranioplasty, surgeons consider the size and location of the defect, the patient's overall health, and the specific advantages and disadvantages of each material. The goal is to choose a material that offers the best combination of durability, biocompatibility, and aesthetic results.
Surgical Procedure for Cranioplasty
1. Anesthesia: Cranioplasty is a significant surgical procedure that often requires precision and can be time-consuming.
- General Anesthesia: Most commonly used for cranioplasty. The patient is rendered unconscious, ensuring they remain still during the operation and feel no pain. Vital signs are continuously monitored, and the patient's airway is often secured using intubation.
- Local Anesthesia: Used in rare cases for smaller procedures or when general anesthesia poses risks. The area around the surgical site is numbed, but the patient remains awake. They might also receive sedation to keep them relaxed.
2. Incision: The surgeon makes an incision over the area of the defect. The location and type of incision depend on the defect's position and size.
- Linear Incision: A straight-line cut, often used for defects located near the midline or for those that are elongated.
- Curved or S-Shaped Incision: These can provide better access for broader or irregularly shaped defects.
3. Preparation of the Defect: Once the skull is exposed, the surgical team proceeds to prepare the defect.
- Cleaning: Any debris, scar tissue, or unhealthy bone edges are removed.
- Shaping: The edges of the defect might be smoothed or contoured to ensure a better fit for the graft or implant.
4. Placement of the Graft or Implant: The chosen material, whether it's an autologous graft, allograft, or synthetic implant, is then placed over the defect.
- Customization: The graft or implant might need to be shaped or trimmed to fit the defect perfectly.
- Fixation: Once in place, the material is secured using various methods. This can include titanium screws, plates, or special adhesives. The goal is to ensure the graft or implant remains stable and integrates well with the surrounding bone.
5. Closure: After the graft or implant is securely in place, the surgical team proceeds to close the incision.
- Layered Closure: Often, the closure is done in layers, starting with the deeper tissues and working outward. This ensures a more secure and aesthetically pleasing result.
- Suturing: The skin is sutured using either absorbable sutures (which dissolve over time) or non-absorbable ones (which might need removal later).
- Dressings: Sterile dressings are applied over the incision to protect it and reduce the risk of infection.
Post-operatively, patients are closely monitored in a recovery room. They might receive pain medications, antibiotics, and specific instructions for wound care. Follow-up visits ensure the graft or implant is integrating well and that there are no complications.
Post-operative Care for Cranioplasty
1. Monitoring: After the surgery, patients are typically observed in a recovery room or intensive care unit, especially if the procedure was extensive.
- Vital Signs: Continuous monitoring of blood pressure, heart rate, oxygen saturation, and respiratory rate to ensure stability.
- Neurological Status: Regular checks for alertness, pupil response, motor function, and sensory function to detect any neurological changes.
- Wound Inspection: The surgical site is inspected for signs of swelling, bleeding, or discharge, which could indicate complications like infection or hematoma.
2. Medications: Various medications are prescribed post-operatively to manage pain, prevent infections, and address other concerns.
- Pain Relief: Analgesics, such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs), are given to manage pain. For more severe pain, opioids might be prescribed but are used cautiously due to their potential for addiction and side effects.
- Antibiotics: Prophylactic antibiotics might be given to prevent infections, especially if synthetic materials were used during the surgery.
- Antiseizure Medications: In some cases, especially if the surgery involved brain manipulation, antiseizure drugs might be prescribed as a precaution.
3. Physical Therapy: While not always necessary, some patients might benefit from rehabilitation post-cranioplasty.
- Mobility Exercises: To prevent muscle stiffness and improve circulation, especially if the patient has been bedridden.
- Strengthening Exercises: To regain muscle strength if there has been any muscle atrophy.
- Neurological Rehabilitation: For patients who have experienced neurological deficits, targeted exercises and therapies can help improve function.
4. Follow-up Visits: Regular check-ups post-surgery are crucial to ensure the patient is healing well and the graft or implant is integrating properly.
- Wound Assessment: The surgical site is inspected for signs of healing, and any non-absorbable sutures might be removed.
- Imaging Studies: CT scans or X-rays might be taken to visualize the graft or implant and ensure it's in the correct position.
- Neurological Checks: Continued assessment of the patient's neurological status to detect any changes or improvements.
- Discussion of Recovery: The surgeon will provide guidelines on activities to avoid, signs of complications to watch for, and expected recovery timelines.
Post-operative care is a critical phase after cranioplasty. Proper care and monitoring ensure that complications are detected early and addressed promptly, leading to better outcomes and faster recovery for the patient.
Complications and Risks of Cranioplasty
1. Infection: Infections can occur at the surgical site or deeper within the skull.
- Signs:
- Redness and warmth at the incision site.
- Swelling or pus discharge.
- Fever and chills.
- Increased pain or tenderness around the surgical area.
- Prevention:
- Sterile surgical techniques.
- Prophylactic antibiotics before and after surgery.
- Proper wound care post-operatively, including keeping the area clean and dry.
- Treatment:
- Oral or intravenous antibiotics, depending on the severity.
- In severe cases, surgical intervention might be required to clean out the infected area.
2. Graft or Implant Failure: The graft or implant might not integrate well with the surrounding bone or could become displaced.
- Causes:
- Poor surgical technique.
- Inadequate fixation during surgery.
- Infection or rejection by the body.
- Trauma or injury post-operatively.
- Solutions:
- Monitoring through imaging studies to detect early signs of failure.
- Surgical revision might be required to replace or reposition the graft or implant.
3. Hematoma: This is a collection of blood at the surgical site, which can increase pressure on the brain.
- Signs:
- Swelling or bulging at the surgical site.
- Pain or increased pressure sensation.
- Neurological symptoms like dizziness, confusion, or weakness.
- Prevention:
- Meticulous surgical technique to ensure all blood vessels are cauterized or sutured.
- Post-operative monitoring to detect early signs.
- Treatment:
- Small hematomas might resolve on their own.
- Larger ones might require surgical drainage to relieve pressure.
4. Neurological Complications: Surgery involving the skull and brain always carries a risk of affecting neurological function.
- Signs:
- Changes in consciousness or alertness.
- New or worsening weakness, numbness, or tingling.
- Vision changes.
- Speech difficulties or confusion.
- Seizures.
- Prevention:
- Careful surgical technique to avoid damaging brain tissue.
- Monitoring during surgery, such as using intraoperative neurophysiological monitoring.
- Treatment:
- The specific treatment depends on the nature of the complication. It might involve medications, further surgeries, or targeted rehabilitation therapies.
While cranioplasty is generally a safe procedure with high success rates, it's essential for patients to be aware of potential complications and risks. Proper pre-operative planning, skilled surgical technique, and vigilant post-operative care can minimize these risks and ensure the best possible outcomes.
Outcomes and Prognosis of Cranioplasty
1. Success Rates: Cranioplasty, with modern surgical techniques and materials, boasts a high success rate. While the exact percentage can vary based on the specific indication for surgery, the surgeon's experience, and the chosen material, many studies report success rates upwards of 90%. This means that the vast majority of patients experience a successful graft or implant integration without major complications.
2. Long-term Outcomes: The durability of the graft or implant is a significant concern for both surgeons and patients.
- Autologous Grafts: These tend to have excellent long-term outcomes, as the bone integrates naturally with the surrounding skull. However, there's a risk of bone resorption over time, especially if the graft was taken from certain areas like the rib.
- Allografts: While they can provide good long-term results, there's a slightly higher risk of complications like infection or graft rejection compared to autologous grafts.
- Synthetic Materials: The durability of synthetic materials like titanium or PMMA is generally excellent. These materials are resistant to wear and tear and can last a lifetime. However, there's always a risk of complications like infection, implant displacement, or, in rare cases, implant degradation.
3. Patient Satisfaction: The goal of cranioplasty is not just to protect the brain but also to restore the skull's natural contour and appearance.
- Cosmetic Results: Most patients report a significant improvement in their appearance post-cranioplasty. The restoration of the skull's shape can have profound effects on self-esteem and social interactions. With custom-made implants or meticulously shaped grafts, the cosmetic results can be impressive.
- Functional Results: Beyond aesthetics, cranioplasty aims to improve brain function by providing a protective barrier and, in some cases, improving cerebral hemodynamics. Many patients experience improved neurological function, reduced symptoms, and an overall better quality of life post-surgery.
In conclusion, the outcomes and prognosis for cranioplasty are generally very positive. With skilled surgical intervention, appropriate post-operative care, and regular follow-ups, most patients can expect excellent cosmetic and functional results that last a lifetime.
Recent Advances and Future Directions in Cranioplasty
1. New Materials: The field of biomaterials has seen rapid advancements, leading to the development of innovative synthetic grafts and implants for cranioplasty.
- Bioactive Ceramics: Materials like bioactive glass and certain ceramic composites have shown promise due to their osteoconductive properties, promoting bone growth and integration.
- Polymer Composites: Combining the strength of traditional materials with the flexibility and biocompatibility of polymers, these composites offer a balance between durability and adaptability.
2. Technological Advancements: Modern technology has revolutionized the way cranioplasty procedures are planned and executed.
- 3D Printing: Custom-made implants can now be created using 3D printing technology. These implants are designed based on the patient's own imaging studies, ensuring a perfect fit and superior cosmetic results.
- Computer-Assisted Surgery: With the help of advanced software, surgeons can plan the procedure in detail, visualizing the placement of the graft or implant and predicting potential challenges.
- Augmented Reality (AR) and Virtual Reality (VR): These technologies can provide real-time guidance during surgery, overlaying digital images on the surgical field and aiding in precision.
3. Research: Ongoing studies are exploring various aspects of cranioplasty, from materials to techniques.
- Biological Integration: Research is focused on improving the integration of grafts and implants with the surrounding tissue, reducing the risk of complications.
- Minimally Invasive Techniques: Studies are exploring ways to perform cranioplasty with smaller incisions and less tissue disruption, leading to faster recovery times.
- Neuroprotective Strategies: Alongside structural repair, research is delving into ways cranioplasty can directly benefit brain health and function.
Cranioplasty, a procedure with ancient roots, has evolved into a sophisticated surgical intervention that offers both functional and cosmetic benefits. The importance of restoring the skull's integrity cannot be overstated, as it provides critical protection to the brain and significantly impacts an individual's quality of life.
With the advent of new materials and cutting-edge technologies, the future of cranioplasty looks promising. As research continues to push the boundaries of what's possible, patients can expect even better outcomes and fewer complications.
However, the success of cranioplasty doesn't solely rest on surgical advancements. Early intervention, thorough pre-operative evaluation, and diligent post-operative care remain crucial components of the process. By combining the best of modern medicine with a comprehensive care approach, cranioplasty will continue to change lives for the better.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!






