
Understanding Cirrhosis and Its Stages: A Comprehensive Guide
19 Oct, 2023
 Healthtrip
HealthtripCirrhosis is a chronic liver disease that affects millions of people worldwide. It is a condition characterized by the gradual and irreversible scarring of the liver tissue, which can lead to a range of complications and, in severe cases, liver failure. In this blog, we will delve into the intricacies of cirrhosis, its causes, symptoms, and stages, to provide a comprehensive understanding of this debilitating condition.
What is Cirrhosis?
Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as hepatitis and chronic alcoholism. The liver carries out several necessary functions, including detoxifying harmful substances in your body, cleaning your blood, and making vital nutrients. Cirrhosis can lead to a number of complications, including liver cancer.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Causes of Cirrhosis
Cirrhosis can develop from various liver diseases and conditions, including:
1. Hepatic Causes
1.1 Chronic Alcohol Consumption (Hepatic): Excessive and prolonged alcohol abuse can lead to alcoholic liver disease, causing inflammation and scarring of the liver tissue, ultimately progressing to cirrhosis.
1.2 Non-Alcoholic Fatty Liver Disease (NAFLD) (Hepatic): NAFLD, often associated with obesity and metabolic syndrome, involves the accumulation of fat in the liver, leading to inflammation and, in some cases, cirrhosis.
2. Hepatitis
2.1 Hepatitis B (Hepatitis): Chronic infection with the hepatitis B virus can result in ongoing liver inflammation and fibrosis, ultimately leading to cirrhosis.
2.2 Hepatitis C (Hepatitis): Chronic infection with the hepatitis C virus is a common cause of cirrhosis. The virus attacks the liver, causing persistent inflammation and damage.
3. Hereditary
3.1 Hemochromatosis (Hereditary): Hemochromatosis is a hereditary condition that causes the body to absorb excess iron from the diet. Over time, this iron accumulates in the liver, leading to cirrhosis.
Most popular procedures in India
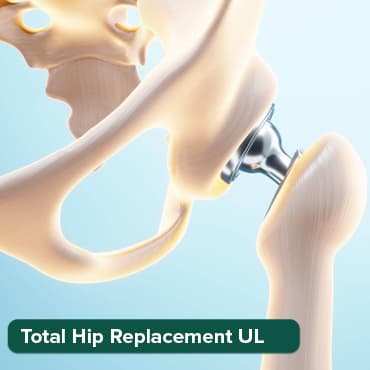
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
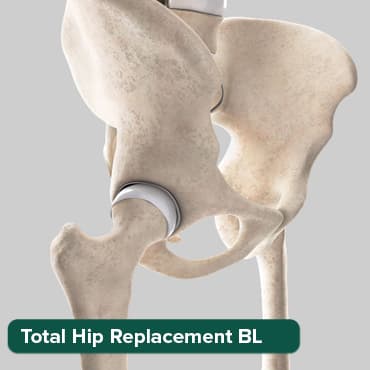
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ANGIOGRAM
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

3.2 Wilson's Disease (Hereditary): Wilson's disease is a genetic disorder that causes the buildup of copper in the liver. If left untreated, it can lead to cirrhosis and other complications.
4. Hemochromatosis
4.1 Hemochromatosis (Hemochromatosis): As mentioned above, hemochromatosis is a condition that can lead to cirrhosis by causing excess iron to accumulate in the liver.
5. Harmful Substances
5.1 Medications (Harmful Substances): Prolonged use of certain medications, such as methotrexate or isoniazid, can lead to drug-induced liver injury and cirrhosis.
5.2 Environmental Toxins (Harmful Substances): Exposure to certain environmental toxins, such as industrial chemicals and aflatoxins (produced by molds), can damage the liver and contribute to cirrhosis.
Symptoms of Cirrhosis
Cirrhosis often progresses slowly and may not cause any symptoms in its early stages. As the disease advances, the following symptoms and complications can occur:
1. Hepatic Symptoms
1.1 Jaundice (Hepatic): One of the most noticeable symptoms of cirrhosis is jaundice. The liver's reduced ability to process bilirubin leads to a yellowing of the skin and eyes.
1.2 Fatigue (Hepatic): Individuals with cirrhosis often experience persistent fatigue and weakness, which can be attributed to the liver's decreased capacity to metabolize nutrients and remove toxins.
1.3 Itchy Skin (Hepatic): The buildup of bile products in the bloodstream can result in intense itching of the skin.
2. Hemodynamic Symptoms
2.1 Ascites (Hemodynamic): Cirrhosis can lead to the accumulation of fluid in the abdominal cavity, known as ascites. This can cause abdominal discomfort, swelling, and increased abdominal girth.
2.2 Edema (Hemodynamic): Swelling, particularly in the legs and ankles (edema), is another common symptom of cirrhosis, stemming from the liver's impaired ability to regulate fluid balance.
2.3 Enlarged Spleen (Hemodynamic): As cirrhosis progresses, the spleen can become enlarged, leading to a sense of fullness or discomfort in the upper left abdomen.
3. Hematologic Symptoms
3.1 Easy Bruising and Bleeding (Hematologic): The liver's reduced production of blood-clotting proteins can result in easy bruising and prolonged bleeding, even from minor cuts and injuries.
3.2 Anemia (Hematologic): Cirrhosis can lead to anemia due to a decreased production of red blood cells. Anemia can cause weakness and fatigue.
3.3 Petechiae (Hematologic): Tiny, red or purple dots on the skin, known as petechiae, can develop due to low platelet counts associated with cirrhosis.
Stages of Cirrhosis
Cirrhosis is often classified into different stages based on the extent of liver damage. This helps doctors understand the severity of the condition and determine appropriate treatment options. The most commonly used classification is the Child-Pugh score and the Model for End-Stage Liver Disease (MELD) score.
1. Hepatic Parameters
1.1 Bilirubin Levels (Hepatic): One of the components of the Child-Pugh score is bilirubin levels, which serve as a measure of liver function. Elevated bilirubin levels can indicate impaired liver function, often seen in cirrhosis.
1.2 Albumin Levels (Hepatic): Albumin is a protein produced by the liver. Low levels of albumin in the blood can be a sign of liver dysfunction and are considered in the Child-Pugh score.
2. Prothrombin Time
2.1 Prothrombin Time (Coagulation): Prothrombin time is a measure of blood clotting. In cirrhosis, the liver's ability to produce clotting factors is impaired, leading to prolonged prothrombin time. This parameter is included in the Child-Pugh score to assess the severity of the coagulation abnormalities.
3. Ascites
3.1 Ascites (Ascites): The presence of fluid in the abdominal cavity, known as ascites, is considered in the Child-Pugh score. Ascites is a common complication of cirrhosis and reflects the extent of liver decompensation.
4. Hepatic Encephalopathy
4.1 Hepatic Encephalopathy (Encephalopathy): Brain dysfunction due to liver disease, known as hepatic encephalopathy, is another important component of the Child-Pugh score. It reflects the impact of liver dysfunction on neurological function.
The Child-Pugh score is a valuable tool for assessing the severity of cirrhosis and helps categorize patients into different classes, ranging from Class A (less severe) to Class C (most severe). This classification aids in making treatment decisions and predicting outcomes in individuals with cirrhosis.
Model for End-Stage Liver Disease (MELD) Score
The MELD score uses laboratory values, including creatinine, bilirubin, and international normalized ratio (INR), to assess the severity of cirrhosis. A higher MELD score indicates a higher risk of mortality, and it is often used to prioritize patients for liver transplantation.
Treatment and Management
The treatment of cirrhosis varies depending on the underlying cause and the stage of the disease. Some general approaches include:
1. Hepatic Management
1.1 Liver Transplant (Hepatic): In cases of severe cirrhosis where the liver has significantly deteriorated, a liver transplant may be the only viable option. A transplant involves replacing the damaged liver with a healthy one from a living or deceased donor.
1.2 Management of Complications (Hepatic): Treating complications associated with cirrhosis, such as ascites, hepatic encephalopathy, variceal bleeding, and hepatocellular carcinoma, is a crucial aspect of hepatic management.
2. Lifestyle Modifications
2.1 Alcohol Abstinence (Lifestyle Modifications): For individuals with alcoholic cirrhosis, complete abstinence from alcohol is essential to prevent further liver damage. Support groups and counseling can be beneficial in maintaining sobriety.
2.2 Dietary Changes (Lifestyle Modifications): A balanced diet that is low in sodium can help manage ascites and fluid retention. Proper nutrition is essential to address malnutrition, a common issue in cirrhosis patients.
2.3 Weight Management (Lifestyle Modifications): For individuals with non-alcoholic fatty liver disease (NAFLD), losing excess weight through a balanced diet and exercise is crucial to prevent cirrhosis.
3. Medications
3.1 Medications (Medications): Medications may be prescribed to manage various symptoms and complications of cirrhosis. These may include diuretics to reduce fluid buildup, beta-blockers to manage portal hypertension, and lactulose to treat hepatic encephalopathy.
3.2 Antiviral Medications (Medications): In the case of cirrhosis caused by viral hepatitis (such as hepatitis B or C), antiviral medications may be prescribed to control the viral infection and prevent further liver damage.
4. Monitoring
4.1 Regular Check-ups (Monitoring): Individuals with cirrhosis require regular follow-up appointments with healthcare providers. These visits are essential to monitor liver function, assess for complications, and adjust treatment plans as necessary.
Complications of Cirrhosis
1. Hepatic Complications
1.1 Portal Hypertension (Hepatic): Cirrhosis often leads to increased pressure in the portal vein, resulting in portal hypertension. This condition can lead to the development of enlarged blood vessels (varices) in the esophagus and stomach, which can rupture and cause life-threatening bleeding.
1.2 Ascites (Hepatic): Ascites is the accumulation of fluid in the abdominal cavity, often due to impaired blood flow through the liver. It can lead to abdominal discomfort, difficulty breathing, and an increased risk of infection.
1.3 Hepatic Encephalopathy (Hepatic): Hepatic encephalopathy is a condition in which toxins build up in the bloodstream and affect brain function. It can range from mild confusion to severe disorientation and coma.
2. Hemodynamic Complications
2.1 Hepatorenal Syndrome (Hemodynamic): Cirrhosis can lead to hepatorenal syndrome, a condition in which kidney function is compromised. This condition is characterized by decreased urine output and increased creatinine levels, and it requires immediate medical attention.
2.2 Spontaneous Bacterial Peritonitis (Hemodynamic): Individuals with cirrhosis are at an increased risk of developing spontaneous bacterial peritonitis, an infection in the ascitic fluid. This condition is a serious complication of ascites and requires antibiotic treatment.
3. Hematologic Complications
3.1 Coagulopathy (Hematologic): Cirrhosis often results in coagulation abnormalities due to decreased production of clotting factors by the liver. This can lead to easy bruising and bleeding.
3.2 Anemia (Hematologic): Cirrhosis can cause anemia due to decreased production of red blood cells. Anemia leads to weakness and fatigue.
4. Hepatocellular Complications
4.1 Hepatocellular Carcinoma (Hepatocellular): Long-term cirrhosis increases the risk of developing hepatocellular carcinoma (HCC), a form of liver cancer. Regular monitoring and screening are essential for early detection of HCC.
4.2 Liver Failure (Hepatocellular): In advanced stages of cirrhosis, the liver's function deteriorates to the point of liver failure. This is a life-threatening condition, and the only effective treatment is a liver transplant.
Prevention and Lifestyle Modifications
1. Hepatic Prevention
1.1 Limit Alcohol Consumption (Hepatic): To prevent alcoholic liver disease and cirrhosis, individuals should practice moderate or complete abstinence from alcohol, depending on their risk factors and history of alcohol abuse.
1.2 Non-Alcoholic Fatty Liver Disease (Hepatic): For those at risk of non-alcoholic fatty liver disease (NAFLD), maintaining a healthy weight through a balanced diet and regular exercise can help prevent cirrhosis.
2. Hepatitis Prevention
2.1 Safe Sex and Hepatitis Vaccination (Hepatitis): Practicing safe sex and getting vaccinated against hepatitis B can help prevent viral hepatitis infections, which are common causes of cirrhosis.
2.2 Hepatitis C Screening (Hepatitis): Periodic screening for hepatitis C is essential for early detection and treatment, which can prevent cirrhosis in individuals with the virus.
3. Healthy Living
3.1 Weight Management (Healthy Living): Maintaining a healthy weight through proper nutrition and exercise can help prevent non-alcoholic fatty liver disease and cirrhosis.
3.2 Balanced Diet (Healthy Living): Consuming a diet that is low in saturated fats, sugars, and salt, and rich in fruits, vegetables, and whole grains is beneficial for liver health.
4. Avoiding Harmful Substances
4.1 Safe Medication Use (Harmful Substances): Individuals should take medications as prescribed and avoid overusing or misusing drugs, especially those known to cause liver damage.
4.2 Avoid Sharing Needles (Harmful Substances): Individuals using injectable drugs should never share needles, as this can transmit infections that lead to cirrhosis.
5. Hepatitis Vaccination
5.1 Hepatitis Vaccination (Hepatitis Vaccination): Getting vaccinated against hepatitis A and B can provide effective prevention against these viral infections, reducing the risk of hepatitis-related cirrhosis.
Support and Lifestyle Management
Living with cirrhosis can be challenging, but with the right support and lifestyle adjustments, individuals can lead fulfilling lives. Here are some important considerations:
- Dietary Changes: A balanced diet low in sodium is essential to manage ascites and fluid retention. Protein intake may need to be adjusted under the guidance of a healthcare provider to prevent encephalopathy. Nutritional support is crucial, as malnutrition is common in cirrhotic patients.
- Medication Adherence: If you've been prescribed medications to manage cirrhosis-related complications, it's crucial to take them as directed. These may include diuretics, beta-blockers, or lactulose to manage various symptoms.
- Regular Check-ups: Routine follow-up appointments with your healthcare provider are necessary to monitor liver function, assess for complications, and adjust treatment plans as needed.
- Alcohol Abstinence: If alcohol is a contributing factor to your cirrhosis, complete abstinence is essential. Support groups and counseling can be valuable in maintaining sobriety.
- Mental Health Support: Living with a chronic illness like cirrhosis can be emotionally challenging. Seek out mental health support when needed to address stress, anxiety, and depression.
- Exercise: Regular physical activity can improve overall health and help manage complications such as muscle wasting. Consult your healthcare provider before starting an exercise regimen.
- Liver Transplant Evaluation: For individuals with advanced cirrhosis, a liver transplant may be the only option. Consultation with a transplant center is crucial to assess eligibility and get on the transplant waiting list.
The Role of Family and Caregivers
Cirrhosis often affects not only the individual but also their family and caregivers. Here are some ways loved ones can provide support:
- Educate Yourself: Understand cirrhosis, its stages, and treatment options to better support your loved one.
- Emotional Support: Cirrhosis can be emotionally taxing. Be a source of emotional support and encouragement.
- Assist with Medications: Help ensure that medications are taken as prescribed and that healthcare appointments are kept.
- Maintain a Healthy Lifestyle: Encourage a healthy diet and lifestyle for the individual with cirrhosis.
- Be Vigilant: Watch for signs of complications or symptom exacerbation and seek medical attention promptly when necessary.
- Join a Support Group: Consider joining a support group for caregivers to connect with others in similar situations and share experiences.
In Conclusion
Cirrhosis is a complex and progressive condition that affects the liver and, in many cases, the entire life of an individual. Understanding its causes, symptoms, stages, and management options is crucial for both patients and their loved ones. With proper medical care, lifestyle adjustments, and emotional support, individuals with cirrhosis can maintain a good quality of life and manage the condition effectively. If you or someone you know is affected by cirrhosis, seeking help from healthcare professionals, support groups, and counselors is a positive step towards improved well-being. Remember, with timely intervention and the right approach, cirrhosis can be managed and its impact minimized
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!
