
Treatment Options for Cervical Cancer
04 Dec, 2023
 Healthtrip Team
Healthtrip TeamCervical cancer is a formidable medical challenge, presenting a significant threat to the health and well-being of women worldwide. This diagnosis often engenders fear, uncertainty, and a multitude of questions concerning the most effective course of action for treatment.
The intricate landscape of cervical cancer treatment can be profoundly daunting, leaving patients and their families grappling with feelings of vulnerability. The complexity of the disease and the uncertainty surrounding treatment options can be emotionally taxing, necessitating a clear and informed path forward.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

In this comprehensive blog, we shall address these concerns comprehensively, offering an in-depth exploration of the three primary treatment modalities for cervical cancer: surgery, radiation therapy, and chemotherapy. By gaining a profound understanding of these treatment options, patients and their families can be equipped with the knowledge needed to make informed, empowered decisions as they navigate the challenges associated with this serious medical condition.
Symptoms of Cervical cancer
1. Abnormal Vaginal Bleeding:
- Unusual bleeding between menstrual periods.
- Bleeding after sexual intercourse.
- Heavier or longer menstrual periods than usual.
- Postmenopausal bleeding, which should never occur and should always be investigated.
2. Pelvic Pain:
- Persistent, unexplained pain in the pelvis or lower abdomen.
- Discomfort during sexual intercourse.
3. Unusual Vaginal Discharge:
An increase in vaginal discharge that may be watery, bloody, or foul-smelling.
4. Pain During Urination:
Most popular procedures in India
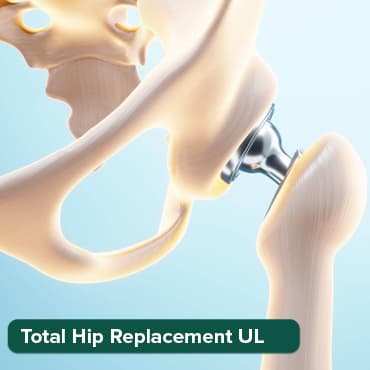
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
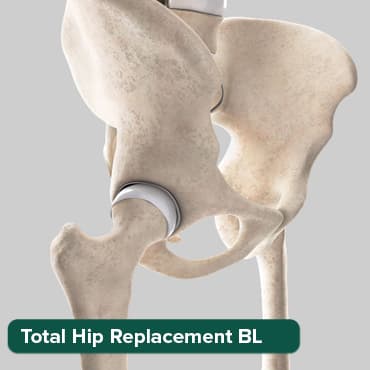
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ANGIOGRAM
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

Pain or discomfort while urinating.
5. Leg Swelling:
Swelling in one or both legs due to impaired blood flow (a less common symptom, associated with more advanced stages).
6. Back Pain or Bone Pain:
Pain in the back or pelvis that may be caused by the cancer spreading to nearby tissues or bones.
7. Weight Loss and Fatigue:
- Unexplained weight loss.
- Persistent fatigue and weakness, which may be associated with advanced cervical cancer.
8. Recurrent Urinary Tract Infections (UTIs):
Frequent UTIs or bladder infections may be a symptom of cervical cancer in some cases.
A. Surgery
a. Cone Biopsy (LEEP) for Cervical Cancer
Cone biopsy, medically known as Loop Electrosurgical Excision Procedure (LEEP), is a surgical procedure often employed in the management of cervical cancer and cervical intraepithelial neoplasia (CIN). It serves both diagnostic and therapeutic purposes and is typically recommended when cancer is confined to the cervix or when abnormal cervical cells require removal.
Purpose:
- Diagnosis: To confirm the presence of cervical cancer or assess the extent of precancerous lesions when abnormal cells are detected during cervical cancer screening tests like Pap smears or colposcopies.
- Treatment (Therapeutic): In cases of early-stage cervical cancer or precancerous lesions, cone biopsy can serve as a therapeutic procedure by removing the cancerous or abnormal tissue, effectively treating the disease or preventing its progression.
- Staging: To determine the stage of cervical cancer and help guide further treatment decisions by evaluating the extent of the disease.
Procedure of Cone Biopsy (LEEP):
The steps involved in a cone biopsy procedure, also known as LEEP, are as follows:
1. Preparation: The patient is prepared for the procedure, usually as an outpatient, with local anesthesia applied to the cervix to numb the area. In some cases, a mild sedative may be administered to relax the patient.
2. Instrumentation: A specialized instrument, known as a LEEP electrode or loop, is used. It consists of a thin wire loop that carries an electrical current. This loop is inserted through the vagina and positioned around the abnormal tissue on the cervix.
3. Excision: The surgeon activates the electrical current, which heats the wire loop. The loop is then used to cut away a cone-shaped piece of cervical tissue that includes the abnormal cells or cancerous tissue.
4. Hemostasis: The electrical current also cauterizes (seals) the blood vessels as the tissue is removed, minimizing bleeding during and after the procedure.
5. Removal and Examination: The excised tissue is sent to a pathology lab for examination to confirm the presence of cancer or precancerous cells and determine the extent of the disease.
6. Recovery: After the procedure, patients typically rest briefly in a recovery area. Mild discomfort and vaginal discharge are common after a cone biopsy, but these symptoms usually resolve within a few weeks.
Risks and Considerations:
While cone biopsy is generally considered safe, it does carry some risks, including bleeding, infection, scarring, and the possibility of incomplete removal of cancerous tissue. Patients should discuss the potential risks and benefits of cone biopsy with their healthcare team to make informed decisions about their treatment.
Cone biopsy (LEEP) is a versatile procedure used both for diagnosis and treatment in cervical cancer management. It is particularly valuable in early-stage disease and for preventing cervical cancer in cases of precancerous lesions. Patients should engage in a thorough discussion with their healthcare providers to determine the most suitable treatment approach based on their specific circumstances.
b. Hysterectomy in Cervical Cancer
A hysterectomy is a surgical procedure that involves the removal of the uterus, and in some cases, additional reproductive organs such as the cervix, ovaries, and fallopian tubes. Hysterectomy is a common treatment option for cervical cancer, particularly in more advanced stages. Here's a detailed overview of why and how it is performed:
Purpose:
- Cancer Removal: To remove the source of cervical cancer, which is the uterus, and potentially other reproductive organs (cervix, ovaries, fallopian tubes) when indicated. This aims to eliminate cancerous tissue and prevent further growth and spread.
- Definitive Treatment: In some cases, hysterectomy serves as the primary treatment for cervical cancer, especially in more advanced stages when other treatments may not be suitable or effective.
- Adjuvant Therapy: After surgery, hysterectomy may be used as adjuvant therapy to reduce the risk of cancer recurrence by removing any remaining cancer cells.
Types of Hysterectomy:
There are different types of hysterectomy procedures, depending on which reproductive organs are removed. These include:
- Total Hysterectomy: This involves the removal of the entire uterus, including the cervix.
- Radical Hysterectomy: In a radical hysterectomy, not only is the uterus removed, but also the cervix, upper part of the vagina, and surrounding tissues. Additionally, nearby lymph nodes may be removed to assess cancer spread.
- Modified Radical Hysterectomy: This is a less extensive procedure than a radical hysterectomy and involves the removal of the uterus, cervix, and possibly nearby lymph nodes, but spares the upper part of the vagina.
Procedure of Hysterectomy:
The procedure for hysterectomy involves the following steps:
1. Preparation: The patient is prepared for surgery, typically under general anesthesia. The healthcare team ensures the patient's comfort and safety.
2. Incision: An incision is made in the abdominal wall, although minimally invasive laparoscopic or robotic-assisted techniques may also be used, which involve smaller incisions. The choice of incision type depends on the specific case and the surgeon's expertise.
3. Organ Removal: Depending on the type of hysterectomy, the surgeon carefully removes the uterus, cervix, and potentially other reproductive organs and surrounding tissues. The blood vessels are usually tied off or sealed to prevent bleeding.
4. Closure: After confirming the complete removal of the intended organs, the incisions are closed, and the patient is taken to the recovery room.
Risks and Considerations:
As with any surgical procedure, hysterectomy carries certain risks, including infection, bleeding, damage to nearby structures, and potential side effects related to the removal of reproductive organs. Patients should thoroughly discuss the risks and benefits of hysterectomy with their healthcare team to make informed decisions about their treatment plan.
Hysterectomy is a significant surgical option in the management of cervical cancer, particularly in advanced stages or when other treatments are not effective. It is essential for patients to have a comprehensive discussion with their healthcare providers to determine the most appropriate treatment approach tailored to their specific circumstances and needs.
c. Lymphadenectomy in Cervical Cancer
Lymphadenectomy, also known as lymph node dissection, is a surgical procedure commonly performed in the treatment of cervical cancer. It involves the removal of lymph nodes from the pelvic and para-aortic regions, followed by examination to determine if the cancer has spread to these lymph nodes. This procedure plays a critical role in staging cervical cancer and planning the appropriate course of treatment.
Purpose:
- Staging: Lymphadenectomy is performed to accurately stage cervical cancer by assessing whether cancer cells have spread to nearby lymph nodes. Accurate staging guides further treatment decisions.
- Treatment Planning: To inform the development of an effective treatment plan. If cancer is detected in the lymph nodes, it may necessitate more aggressive treatments to target any remaining cancer cells.
- Prognosis: Lymph node involvement can impact the patient's prognosis, and the presence or absence of cancer cells in the lymph nodes can affect survival rates and long-term outcomes.
The procedure of Lymphadenectomy:
The procedure for lymphadenectomy in cervical cancer involves several steps:
1. Preparation: The patient is prepared for surgery, which may involve general anesthesia. The surgical team ensures the patient's safety and comfort.
2. Incision: An incision is made in the lower abdomen, allowing access to the pelvic and para-aortic lymph nodes. The size and location of the incision may vary depending on the extent of lymph node dissection needed.
3. Node Dissection: The surgeon carefully identifies and removes lymph nodes from the pelvic and para-aortic areas. These lymph nodes are considered sentinel nodes, which are most likely to be involved if the cancer has spread.
4. Examination: The excised lymph nodes are sent to a pathology lab for examination. A pathologist analyzes the nodes to check for the presence of cancer cells. This examination helps determine the stage of the cancer.
5. Closure: After the lymphadenectomy is completed and the surgeon is satisfied with the removal of lymph nodes, the incision is closed, and the patient is taken to the recovery room.
Risks and Considerations:
While lymphadenectomy is an essential diagnostic and staging procedure, it is not without risks. These risks may include bleeding, infection, and damage to nearby structures. Patients should discuss the potential risks and benefits of lymphadenectomy with their healthcare team and ensure they are well-informed before consenting to the procedure.
Lymphadenectomy is a crucial surgical procedure in the management of cervical cancer. It provides valuable information for staging, treatment planning, and prognosis, helping healthcare providers make informed decisions to optimize the patient's care and outcomes.
B. Chemotherapy for Cervical Cancer
Chemotherapy is a vital component of cervical cancer treatment. It involves the use of drugs, referred to as chemotherapy agents, to target and destroy cancer cells or inhibit their growth. Chemotherapy can be employed in various stages and situations of cervical cancer management, either as a standalone treatment or in combination with other therapies. Here's an in-depth overview:
Chemotherapy involves the use of drugs to kill cancer cells or inhibit their growth. It can be used in various stages of cervical cancer, including advanced or recurrent cases. The goals include shrinking tumors, preventing recurrence, or improving symptoms.
Common Chemotherapy Drugs for Cervical Cancer:
Several chemotherapy drugs are used in the treatment of cervical cancer. The choice of drugs and their combination may vary depending on the stage of the cancer and the individual patient's condition. Some common chemotherapy agents for cervical cancer include:
- Cisplatin: Cisplatin is one of the most frequently used chemotherapy drugs for cervical cancer. It works by damaging the DNA in cancer cells, preventing them from dividing and growing.
- Paclitaxel: Paclitaxel is another chemotherapy drug commonly used in cervical cancer treatment. It interferes with the microtubules in cancer cells, disrupting cell division and growth.
- Topotecan: Topotecan is sometimes used when other chemotherapy agents are not effective. It inhibits DNA repair in cancer cells, ultimately leading to cell death.
Procedure of Chemotherapy:
The administration of chemotherapy for cervical cancer involves the following steps:
1. Treatment Plan: A medical oncologist determines the most appropriate chemotherapy regimen based on the patient's cancer stage, overall health, and individual factors.
2. Drug Administration: Chemotherapy drugs can be administered in various ways:
- Intravenous (IV): The drugs are delivered directly into a vein through an IV line.
- Oral: Some chemotherapy drugs are available in pill form and can be taken orally.
- Intramuscular (IM) or Subcutaneous (SC): In some cases, chemotherapy may be injected into a muscle or under the skin.
3. Treatment Schedule: Chemotherapy is typically administered in cycles, with each cycle consisting of a period of drug administration followed by a rest period. The specific schedule and duration depend on the treatment plan.
4. Monitoring and Adjustments: During treatment, the medical team closely monitors the patient's response and may make adjustments to the chemotherapy regimen if necessary.
Risks and Considerations:
Chemotherapy can cause a range of side effects, including fatigue, nausea, vomiting, hair loss, and lowered blood cell counts. The specific side effects and their severity may vary among patients. Managing these side effects is an integral part of cancer care, and patients receive supportive care to minimize discomfort and maintain their quality of life during treatment.
Chemotherapy is a valuable treatment option for cervical cancer, especially in advanced stages or when combined with radiation therapy or as an adjuvant therapy after surgery. Patients should have open and thorough discussions with their healthcare team to understand the treatment plan, potential side effects, and any supportive care measures to optimize their treatment experience and outcomes.
C. Radiation Therapy for Cervical Cancer
Radiation therapy is a crucial treatment option for cervical cancer. It involves the use of high-energy rays or particles to target and destroy cancer cells or shrink tumors. Radiation therapy is typically employed when surgery is not an option or as an adjuvant treatment alongside surgery, chemotherapy, or both. There are two primary types of radiation therapy used in the management of cervical cancer:
a. External Beam Radiation:
External beam radiation therapy (EBRT) is a non-invasive treatment that delivers radiation from outside the body. It is commonly used in cervical cancer treatment and plays a vital role in both curative and palliative care. Here's a detailed look at EBRT:
To target and deliver radiation to the cervix and surrounding tissues from outside the body. This treatment is used to shrink tumors, control cancer growth, or provide palliative care. It may be used alone or in combination with other treatments.
The procedure of External Beam Radiation:
1. Treatment Planning: Prior to treatment, a comprehensive evaluation is performed to determine the precise location of the tumor and the required radiation dose. Specialized imaging, such as CT scans and MRI, may be used for treatment planning.
2. Daily Treatment Sessions: Patients typically undergo daily treatment sessions, Monday through Friday, for several weeks. During each session, the patient lies on a treatment table, and a machine called a linear accelerator delivers high-energy X-ray beams to the targeted area.
3. Precise Targeting: The radiation therapy team takes great care to ensure that the radiation is precisely focused on the cervix and surrounding tissues while minimizing exposure to healthy tissue.
Monitoring and Adjustments: Throughout the course of treatment, the radiation oncologist closely monitors the patient's progress and may make adjustments to the treatment plan if necessary.
b. Brachytherapy:
Brachytherapy is another vital component of radiation therapy for cervical cancer. It involves placing a radioactive source directly inside or very close to the cervix to deliver a high dose of radiation precisely to the cancerous area. Here's a closer look at brachytherapy:
To deliver a high dose of radiation directly to the cervix or nearby tissues by placing a radioactive source inside the body. Brachytherapy is used to treat localized cervical cancer, provide a radiation "boost" in combination with external beam radiation, and improve treatment precision.
Procedure of Brachytherapy:
1. Placement of Radiation Source: During a brachytherapy session, a radioactive source, such as a small tube or seeds, is inserted into the vagina and positioned near the cervix. The source is temporarily placed and remains in the body for a specified period.
2. Precise Delivery: The radioactive source delivers a high dose of radiation directly to the tumor, sparing healthy surrounding tissues.
3. Multiple Sessions: Patients often undergo several sessions of brachytherapy over the course of a few weeks, with each session lasting a few minutes.
4. Close Monitoring: The radiation oncologist closely monitors the patient during and after each session to ensure accurate placement and treatment efficacy.
Risks and Considerations:
Both external beam radiation and brachytherapy have potential side effects, including fatigue, skin irritation, gastrointestinal issues, and urinary symptoms. The specific side effects and their severity vary from patient to patient.
Radiation therapy, including external beam radiation and brachytherapy, is a crucial component of cervical cancer treatment. The choice of radiation therapy and its timing depend on the stage and extent of the cancer, overall health of the patient, and treatment goals. It is essential for patients to have thorough discussions with their healthcare team to understand the treatment plan and potential side effects fully.
D. Immunotherapy for Cervical Cancer
Immunotherapy represents an innovative and promising treatment strategy in the fight against cervical cancer. It is designed to harness the power of the body's immune system to recognize and target cancer cells. Immunotherapy has shown significant potential in the treatment of various cancers, including advanced cervical cancer. Two notable immunotherapy drugs in the context of cervical cancer are pembrolizumab and nivolumab. Here's a comprehensive guide to understand how immunotherapy works and its role in cervical cancer treatment:
Immunotherapy aims to boost the body's immune system to recognize and attack cancer cells. In advanced cervical cancer, drugs like pembrolizumab and nivolumab target immune checkpoints, enabling the immune system to target cancer cells more effectively. Immunotherapy is often used when other treatments have failed.
Immunotherapy Mechanism in Cervical Cancer:
Immunotherapy operates on the principle of enhancing the body's natural defense mechanisms, particularly the immune system, to recognize and attack cancer cells. In the context of cervical cancer, the immune system may not always effectively recognize cancer cells due to various factors. Immunotherapy drugs, such as pembrolizumab and nivolumab, work by blocking specific proteins that inhibit the immune system's response. These proteins, called immune checkpoints, prevent the immune system from attacking normal cells. By blocking these checkpoints, immunotherapy enables the immune system to target and destroy cancer cells more effectively.
Pembrolizumab and Nivolumab:
Pembrolizumab and nivolumab are two immunotherapy drugs that have demonstrated promising results in clinical trials for advanced cervical cancer:
- Pembrolizumab: Pembrolizumab is a checkpoint inhibitor that targets the PD-1 protein on immune cells. By blocking PD-1, pembrolizumab helps unleash the immune system's ability to recognize and attack cancer cells. It has shown efficacy in certain cases of advanced cervical cancer, particularly when the cancer has progressed after standard treatments.
- Nivolumab: Nivolumab is another checkpoint inhibitor that targets the PD-1 protein. It works similarly to pembrolizumab by enhancing the immune system's response against cancer cells. Nivolumab has also demonstrated promise in clinical trials for advanced cervical cancer.
Procedure of Immunotherapy:
Immunotherapy is administered through intravenous (IV) infusions or injections, typically in an outpatient setting. The treatment schedule and duration depend on the specific immunotherapy drug, the patient's response, and the treatment plan.
Risks and Considerations:
While immunotherapy offers the potential for durable responses and fewer side effects compared to traditional chemotherapy, it can still cause immune-related side effects, including fatigue, skin rashes, diarrhea, and inflammation of various organs. Patients receiving immunotherapy are closely monitored, and any side effects are managed promptly.
Immunotherapy represents a promising frontier in cervical cancer treatment, offering new hope to patients with advanced or recurrent disease. Patients should discuss the potential benefits, risks, and specific immunotherapy options with their healthcare team to determine the most appropriate treatment plan tailored to their individual circumstances.
E. Targeted Therapy for Cervical Cancer: Precision Medicine in Action
Targeted therapy is a revolutionary approach to cancer treatment that focuses on specific molecules or pathways involved in the growth and spread of cancer cells. Unlike traditional chemotherapy, which broadly affects both healthy and cancerous cells, targeted therapy aims to selectively target cancer cells while minimizing damage to healthy tissue. In the context of cervical cancer, targeted therapy may be considered when other treatments have not been effective, and it holds promise in improving treatment outcomes. Bevacizumab is one of the targeted therapy drugs used in the treatment of cervical cancer.
Targeted therapy drugs are designed to specifically target molecules or pathways involved in cancer cell growth. In cervical cancer, drugs like bevacizumab are used to disrupt the tumor's blood supply (angiogenesis inhibition) and slow tumor growth. Targeted therapy is typically considered when other treatments have not been effective.
Mechanism of Targeted Therapy:
Targeted therapy drugs work by interfering with specific molecules or pathways that play a crucial role in the survival, growth, and spread of cancer cells. These drugs are designed to block or inhibit these molecules, disrupting the cancer's ability to thrive. In cervical cancer, targeted therapy focuses on molecules or pathways that are particularly relevant to the disease's progression.
Bevacizumab in Cervical Cancer:
Bevacizumab is an example of a targeted therapy drug used in the treatment of cervical cancer. It specifically targets vascular endothelial growth factor (VEGF), a protein that promotes the growth of blood vessels in tumors. By blocking VEGF, bevacizumab inhibits the formation of new blood vessels (angiogenesis) within the tumor, thereby limiting its blood supply and slowing down its growth.
Procedure of Targeted Therapy:
Targeted therapy is typically administered intravenously through regular infusions or injections. The treatment schedule and duration are determined by the specific targeted therapy drug, the patient's response, and the overall treatment plan.
Risks and Considerations:
Targeted therapy drugs can have side effects, which may include high blood pressure, bleeding or clotting problems, gastrointestinal issues, and wound-healing complications. Patients receiving targeted therapy are closely monitored, and any side effects are managed promptly.
Targeted therapy represents an exciting and promising approach to cervical cancer treatment, especially when standard treatments have proven ineffective. Patients should have thorough discussions with their healthcare team to understand the potential benefits, risks, and specific targeted therapy options available to them, as well as how it fits into their overall treatment plan.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!
