
Multiple sclerosis (MS): Types, Symptoms, and Treatment and more
10 Oct, 2023
 Healthtrip Team
Healthtrip TeamLet's explore the intricate landscape of Multiple Sclerosis (MS), where each chapter unfolds a unique story of resilience and hope. From understanding the diverse types to decoding the subtle nuances of symptoms and exploring cutting-edge treatments, join us in unraveling the mysteries of MS and empowering a future filled with knowledge, compassion, and breakthroughs. Welcome to a space where awareness meets possibility–welcome to the world of Multiple Sclerosis
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Multiple sclerosis (MS)
Multiple sclerosis (MS) is a chronic neurological disorder that affects the central nervous system, which includes the brain and spinal cord. It is characterized by inflammation, demyelination (damage to the protective covering of nerve fibers called myelin), and the formation of scar tissue. These processes disrupt the normal flow of electrical impulses along the nerves, leading to a wide range of symptoms.
Types of Multiple sclerosis (MS)
A. Relapsing-Remitting MS (RRMS):
This is the most common form of MS. Individuals with RRMS experience periods of new or worsening symptoms, known as relapses, followed by periods of partial or complete recovery, referred to as remissions. It's like a series of peaks and valleys in the journey of symptoms, making it somewhat unpredictable.
Most popular procedures in
Laparoscopic Cystect
Upto 80% off
90% Rated
Satisfactory
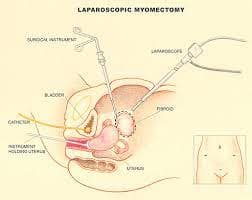
Laparoscopic Myomect
Upto 80% off
90% Rated
Satisfactory

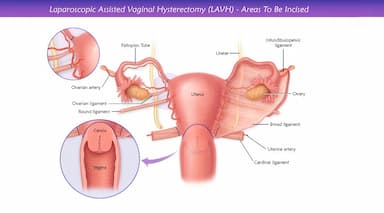
LAVH
Upto 80% off
90% Rated
Satisfactory
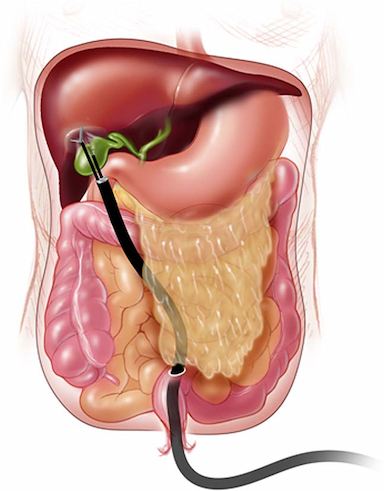
NOTE
Upto 80% off
90% Rated
Satisfactory
CABG
Upto 80% off
90% Rated
Satisfactory
B. Primary Progressive MS (PPMS):
Now, imagine a more gradual and steady progression of symptoms without distinct relapses or remissions. That's the hallmark of PPMS. This type is less common and tends to be diagnosed a bit later in life. Managing PPMS involves addressing the ongoing progression of symptoms rather than navigating through distinct episodes.
C. Secondary Progressive MS (SPMS):
SPMS is often a later stage that follows an initial period of RRMS. In this phase, the disease transitions into a more progressive course, with or without occasional relapses. It's like moving from a rollercoaster ride to a more steadily ascending slope. The transition can vary from person to person.
D. Progressive-Relapsing MS (PRMS):
This is the least common type, presenting a combination of steady progression from the beginning, along with occasional relapses. It's a bit like a tandem dance between continuous symptoms and intermittent exacerbations.
Who Gets Multiple Sclerosis?
A. Age and Gender Distribution:
- Typically diagnosed in early adulthood, between the ages of 20 and 50.
- Women are more commonly affected than men, with a ratio of about 3 to 1.
B. Geographical Patterns:
- Higher prevalence in temperate climates, farther from the equator.
- Varied prevalence rates across different regions, suggesting a potential role of environmental factors.
Symptoms and Signs
A. Neurological Symptoms:
- Fatigue: Persistent and often overwhelming tiredness.
- Motor Issues: Weakness, difficulty with coordination, and problems with balance.
- Sensory Disturbances: Numbness, tingling, or pain.
- Vision Problems: Blurred vision, double vision, or eye pain.
B. Common Signs of MS:
- Lesions on the Central Nervous System: Detected through MRI scans.
- Lesions disrupt the normal flow of electrical impulses in the nervous system.
C. Variability of Symptoms:
- MS is highly individualized; symptoms can range from mild to severe.
- Symptoms may come and go, making the course of the disease unpredictable.
Causes of Multiple Sclerosis
A. Autoimmune Theories:
- The immune system mistakenly attacks the myelin sheath, the protective covering of nerve fibers.
- Inflammation and demyelination result, affecting nerve signal transmission.
B. Genetic Factors:
- Family history may increase the risk, but it's not a strict determinant.
- Certain genetic variations linked to susceptibility.
C. Environmental Triggers:
- Viral infections: Some infections may contribute to the development of MS.
- Vitamin D deficiency: Being in regions with less sunlight exposure is associated with higher risk.
Diagnosis
A. Clinical Evaluation:
- Patient History: Gathering a detailed history, including the onset and progression of symptoms.
- Neurological Examination: Assessing reflexes, coordination, and other neurological functions.
- Elimination of Other Conditions: Ruling out other possible causes of symptoms.
B. Magnetic Resonance Imaging (MRI):
- Visualization of Lesions: Detecting and locating lesions or areas of demyelination in the central nervous system.
- Monitoring Disease Activity: Periodic MRIs help track the progression of the disease.
C. Lumbar Puncture (Spinal Tap):
- Cerebrospinal Fluid Examination: Analyzing the fluid around the spinal cord for abnormalities, such as elevated white blood cells or proteins.
- Detection of Oligoclonal Bands: Presence of specific proteins indicative of an immune response in the central nervous system.
D. Evoked Potentials:
- Measuring Nerve Impulse Response: Recording electrical activity in response to stimuli (visual, auditory, or sensory).
- Identification of Slowed Responses: Assessing delays in nerve signal transmission.
Treatment
A. Disease-Modifying Therapies (DMTs):
- Immunomodulation: Modifying the immune system's response to reduce inflammation and slow disease progression.
- Interferons, glatiramer acetate, and newer biologic agents.
B. Symptomatic Treatments:
- Pain Management: Medications for neuropathic pain or muscle spasms.
- Fatigue Management: Lifestyle adjustments, energy conservation techniques, and sometimes medications.
- Bladder and Bowel Management: Medications, behavioral strategies, and in some cases, surgical interventions.
C. Physical and Occupational Therapy:
- Physical Therapy: Exercises to enhance strength, balance, and coordination.
- Occupational Therapy: Strategies to manage daily activities and maintain independence.
- Assistive Devices: Recommending and training on the use of mobility aids or adaptive equipment.
Risk Factors
A. Genetic Predisposition:
- Family history of MS increases susceptibility.
- Certain genetic variations associated with a higher risk.
B. Environmental Factors:
- Geographical Location: Higher prevalence in regions farther from the equator.
- Sunlight Exposure: Reduced exposure linked to vitamin D deficiency and increased risk.
C. Viral Infections:
- Some viral infections, like Epstein-Barr virus, may be linked to MS development.
- Viral triggers could potentially contribute to the autoimmune response.
Complications
A. Cognitive Impairment:
- Memory loss, difficulty concentrating, and processing information.
- Can range from mild cognitive challenges to more severe impairment.
B. Mobility Issues:
- Weakness, spasticity, and difficulties with coordination.
- Impact on walking, balance, and overall mobility.
C. Emotional and Psychological Impact:
- Depression and Anxiety: Commonly associated with chronic conditions.
- Quality of Life: Affected by the unpredictability of symptoms and the impact on daily activities.
Prevention Strategies
A. Lifestyle Modifications:
- Healthy Diet: Rich in nutrients, particularly vitamin D.
- Regular Exercise: Enhances overall well-being and may help manage symptoms.
B. Immune System Support:
- Adequate sleep, stress management, and a balanced lifestyle to support immune function.
- Consultation with healthcare providers regarding immune-boosting strategies.
C. Early Detection and Intervention:
- Regular health check-ups for early symptom recognition.
- Timely medical intervention, including disease-modifying therapies, to manage and slow progression.
Outlook/Prognosis:
Living with multiple sclerosis (MS) involves a variable course, influenced by factors like disease type and treatment effectiveness. Life expectancy is generally comparable to the general population. However, the focus extends beyond survival to the quality of life, addressing the emotional toll and daily challenges.
In summary, MS is a complex neurological condition with diverse forms and diagnostic approaches. Treatment includes disease-modifying therapies and rehabilitation. Ongoing research promises advancements, offering hope for improved treatments and enhanced quality of life. Collaboration between healthcare professionals, individuals with MS, and researchers continues to drive progress in understanding and managing this condition.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!



