
Epilepsy : Insights into causes, treatment, and daily living
10 Aug, 2023
 Healthtrip Team
Healthtrip TeamWhat is Epilepsy?
Epilepsy, at its core, is a neurological disorder marked by recurrent, unprovoked seizures. These seizures are essentially sudden surges of electrical activity in the brain. But did you know that not all seizures look the same? Epilepsy can be classified into various types based on factors like the origin of the seizure in the brain, awareness during the seizure, and other features.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

How common is Epilepsy?
Globally, epilepsy is more common than one might think. According to the World Health Organization, approximately 50 million people worldwide live with this condition. The demographics of those affected are vast, spanning across age groups, genders, and geographical regions. But why is it essential to understand its prevalence? Because awareness can lead to better support, improved treatments, and a more inclusive society for those living with epilepsy.
Diving into the annals of history, ancient civilizations had varied perceptions of epilepsy. Some viewed it as a divine curse, while others believed it was a form of possession. In ancient Greece, for instance, seizures were sometimes seen as a gift from the gods, a sign of some special connection to the divine.
The journey from ancient beliefs to our current medical understanding of epilepsy is nothing short of fascinating. Over the centuries, as science and medicine progressed, so did our grasp of this condition. By the 19th century, with the advent of modern neurology, epilepsy began to be understood as a disorder of the brain, rather than a supernatural phenomenon. This shift in understanding paved the way for the development of the first antiepileptic drugs and treatments that have since transformed countless lives.
Most popular procedures in India
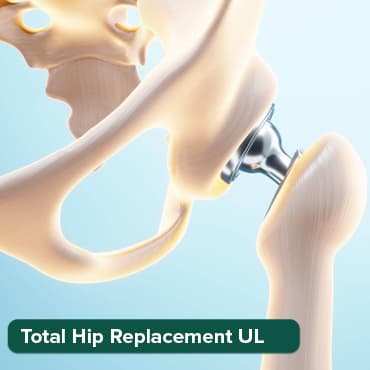
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
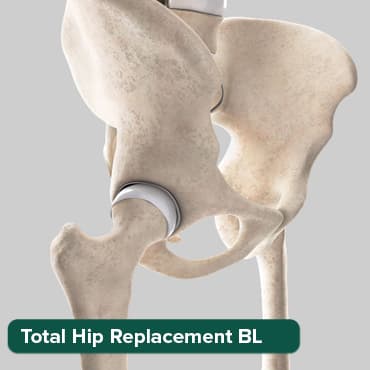
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

Liver Transplant Sur
Upto 80% off
90% Rated
Satisfactory

But this raises a question: If our understanding has evolved so much in the past, what more can we learn about epilepsy in the future?
Etiology: Causes and risk factors
What makes someone prone to epilepsy?
1. Genetic predispositions:
Do you know that our genes can sometimes make us more susceptible to epilepsy? Indeed, certain genetic mutations can increase the risk. While not everyone with these mutations will develop epilepsy, they might have a higher likelihood than the general population.
2. Structural abnormalities:
Brain Malformations and tumors:
The brain's structure plays a pivotal role in its function. So, what happens when there's an anomaly? Malformations from birth or tumors that develop later in life can disrupt the brain's normal electrical activity, leading to seizures.
3. Metabolic and immune disorders:
Our body's metabolism and immune response are like well-oiled machines. But when they malfunction, the repercussions can be vast. Some metabolic disorders can alter the brain's chemical balance, while certain immune disorders might mistakenly attack parts of the brain, both potentially triggering seizures.
4. Infectious agents and Post-Infectious sequelae:
Ever wondered if infections can lead to epilepsy? The answer is, sometimes, yes. Infections like meningitis or encephalitis can directly affect the brain. Moreover, the aftermath of some infections, known as post-infectious sequelae, can also result in epilepsy in some individuals.
5. Traumatic brain injuries and their mechanisms:
Accidents happen. And sometimes, they can lead to traumatic brain injuries (TBIs). Depending on the severity and location of the injury, TBIs can sometimes result in epilepsy. The mechanism? Damage to certain brain regions can alter its electrical activity, leading to seizures.
6. Stroke and vascular causes:
Stroke, a disruption of blood flow to the brain, is a significant risk factor for epilepsy, especially in older adults. But why? When a stroke occurs, it can damage brain tissue, and this damaged area can become a hotspot for seizures. Similarly, other vascular issues in the brain can also pave the way for epilepsy.
In understanding the causes and risk factors, we're better equipped to prevent, diagnose, and treat epilepsy.
Types of Seizures
Seizures can manifest in various ways, depending on which part of the brain they originate from and how they spread. Here's a breakdown of the primary types:
1. Focal (or Partial) seizures:
These seizures start in a specific part of the brain and can remain localized or spread to other areas.
- Simple Partial seizures:
Also known as "focal aware seizures," during these seizures, the person remains conscious and aware. They might experience unusual feelings, sensations, or involuntary movements. - Complex partial seizures:
Now referred to as "focal onset impaired awareness seizures," consciousness is impaired or lost during these seizures. They can involve complex, involuntary behaviors that might seem purposeful but aren't under the person's control.
2. Generalized seizures:
These seizures involve both sides of the brain from the onset. They are characterized by:
- Absence seizures (formerly known as Petit Mal):
These are brief lapses in consciousness where the person might stare blankly or have subtle body movements. They're common in children and can occur multiple times a day. - Tonic seizures:
Here, the muscles stiffen, especially in the back, arms, and legs. It can cause the person to fall to the ground. - Atonic seizures:
Muscle tone is lost, leading to sudden collapses. They're also known as "drop seizures." - Clonic seizures:
Characterized by repeated, rhythmic jerking movements, especially of the arms and face. - Myoclonic seizures:
These involve sudden, brief jerks or twitches of the arms and legs. - Tonic-Clonic Seizures (formerly known as Grand Mal):
These are the most intense type, involving a combination of muscle stiffening and jerking. There's usually a loss of consciousness.
Symptoms of epilepsy
Epilepsy is a diverse neurological condition, and its symptoms can vary widely based on the type of seizure a person experiences. Here's a breakdown of some common symptoms:
1. Uncontrollable jerking movements of the arms and legs:
Often seen in tonic-clonic or myoclonic seizures, these are sudden, involuntary shaking or jerking actions that can be intense and forceful.
2. Temporary confusion:
A brief state of disorientation or confusion can occur, especially during or after a seizure. It's like the brain "resets" itself, and during this period, the person might not be fully aware of their surroundings.
3. Loss of consciousness or awareness:
Common in complex partial seizures and tonic-clonic seizures, the person might black out or have a lapse in awareness, even if they appear to be awake. They might not remember this period once the seizure ends.
4. Psychic symptoms:
These are more abstract and can include feelings of fear, anxiety, déjà vu, or even euphoria. They're often associated with focal seizures and can serve as a warning sign that a larger seizure is imminent.
5. Staring spells:
Typically seen in absence seizures, these involve a sudden lapse in attention. The person might stare blankly into space and be unresponsive. These spells are brief, often lasting only a few seconds, but can occur multiple times a day.
It's essential to recognize that these symptoms can also occur due to other medical conditions. Therefore, a thorough evaluation by a healthcare professional is crucial to confirm an epilepsy diagnosis .
Clinical presentation
When we talk about epilepsy, it's not a one-size-fits-all scenario. The way it presents can vary widely from one individual to another. Let's delve into the diverse world of seizures and their characteristics.
1. Spectrum of seizure types and their characteristics:
Seizures aren't just about dramatic convulsions, as often portrayed in media. They can range from brief lapses in attention to full-body spasms. Understanding this spectrum is crucial for diagnosis and treatment.
2. Focal vs. Generalized seizures:
a. Focal seizures: These originate in just one part of the brain. Did you know that a person might remain conscious during a focal seizure? They might experience unusual feelings, sensations, or movements.
b. Generalized seizures: These involve both sides of the brain from the onset. They can be more intense, often leading to a loss of consciousness. Examples include tonic-clonic seizures, where the body stiffens and then jerks, and absence seizures, characterized by brief staring spells.
3. Motor vs. Non-motor seizures:
- Motor seizures: As the name suggests, these involve motor symptoms. This could mean involuntary jerking movements, muscle stiffening, or even episodes of limpness.
- Non-motor seizures: These are more subtle. They might involve changes in sensation, emotions, or cognition without any overt physical movement.
4. Prodromal symptoms and postictal states:
- Prodromal symptoms: These are warning signs that can precede a seizure by hours or even days. They're like the calm before the storm, with symptoms like mood changes, irritability, or headaches.
- Postictal states: After the storm (or seizure) has passed, individuals might experience confusion, fatigue, or even amnesia. This post-seizure phase can last anywhere from minutes to hours.
5. Associated neurological and systemic manifestations:
Epilepsy doesn't always come alone. Sometimes, it brings along other neurological symptoms like migraines or coordination issues. Moreover, systemic issues, such as gastrointestinal disturbances or respiratory problems, can also accompany certain seizure types.
Recognizing the diverse clinical presentations of epilepsy is paramount. It not only aids in accurate diagnosis but also in understanding the unique challenges each individual might face. But this leads us to wonder: With such varied presentations, how do healthcare professionals decide on the best course of action for each patient?
Diagnostic
Diagnosing epilepsy isn't just about observing a seizure. It's a meticulous process that combines clinical observations with advanced technological tools. Let's explore the various methods professionals use to pinpoint and understand this condition.
1. Clinical evaluation and seizure classification:
A thorough clinical evaluation is the cornerstone of any diagnosis. By listening to patients describe their seizures and observing any physical signs, doctors can classify the type of seizure and its potential origin. But here's a question: How can a patient's description help if they lose consciousness during a seizure? Often, eyewitness accounts or video recordings can fill in the gaps.
2. Electroencephalogram (EEG): Significance and Patterns:
An EEG is like a window into the brain's electrical activity. By placing electrodes on the scalp, doctors can detect abnormal patterns that suggest a predisposition to seizures. But did you know that sometimes, to capture these abnormalities, patients might need prolonged monitoring, sometimes even for days?
3. Neuroimaging: MRI, CT, PET, and SPECT:
- MRI (Magnetic Resonance Imaging): This tool provides detailed images of the brain, helping identify structural abnormalities like tumors or malformations.
- CT (Computed Tomography): A CT scan, often used in emergencies, can quickly detect bleeding or tumors.
- PET (Positron Emission Tomography) and SPECT (Single Photon Emission Computed Tomography): These advanced imaging techniques can pinpoint the exact location of seizure onset in the brain, especially when surgery is being considered.
4. Neuropsychological assessments
Epilepsy can sometimes impact cognitive functions like memory, attention, or problem-solving. Neuropsychological tests delve deep into these areas, providing insights into the brain regions affected and guiding treatment to ensure a holistic approach to patient care.
With these diagnostic tools at their disposal, healthcare professionals can craft a tailored treatment plan for individuals with epilepsy. But it raises a thought: As technology advances, how might our diagnostic capabilities evolve in the future?
Management and therapeutics
Epilepsy, with its diverse presentations, requires a multifaceted approach to management. From medications to surgeries and even dietary interventions, let's delve into the therapeutic landscape of this condition.
1. Antiepileptic drugs (AEDs): Mechanisms, choices, and side effects:
AEDs are the primary line of defense against seizures. They work by altering the electrical activity of the brain, either by reducing the firing of neurons or by increasing inhibitory processes. But with numerous AEDs available, how do doctors choose the right one? The choice often depends on the type of seizure, patient's age, potential side effects, and even coexisting health conditions. Speaking of side effects, while many patients tolerate AEDs well, some might experience dizziness, fatigue, or even mood changes.
2. Surgical Interventions: Candidates, procedures, and outcomes:
Surgery is typically an option when AEDs aren't effective or when a specific, surgically removable brain region is identified as the seizure's origin. But who are the ideal candidates? Those with focal seizures originating from a single area of the brain, especially if that area isn't vital for essential functions like speech or movement.
- Resective surgery: This involves removing the part of the brain where seizures originate. It's fascinating to think that sometimes, only a small portion of the brain needs to be removed to make a significant difference in seizure control.
- Neuromodulation: Techniques like Vagus Nerve Stimulation (VNS) don't directly target the brain. Instead, they modulate its activity. In VNS, a device is implanted under the skin, sending regular pulses to the brain via the vagus nerve, reducing seizure frequency.
3. Dietary therapies: Ketogenic diet, Modified atkins diet:
Absolutely! The Ketogenic Diet, high in fats and low in carbs, has been shown to reduce seizure frequency in some individuals. Similarly, the Modified Atkins Diet, less strict than the ketogenic one, can also be beneficial. But how do they work? These diets alter brain metabolism, potentially stabilizing its electrical activity.
4. Emerging treatments and research:
The world of epilepsy research is ever-evolving. From exploring the potential of genetic therapies to harnessing the power of AI in seizure prediction, the future holds promise. As we continue to understand the brain better, who knows what innovative treatments lie on the horizon?
Managing epilepsy is a journey, often requiring a combination of therapies. With the right approach, many individuals with epilepsy can lead fulfilling, active lives. But it prompts reflection: As we advance in the medical field, how will our approach to epilepsy management transform in the coming decades?
Living with epilepsy: Psychosocial and practical aspects
Beyond the clinical and therapeutic dimensions, epilepsy has profound effects on an individual's daily life. From personal relationships to professional aspirations, let's explore the broader implications of living with this condition.
1. Impact on quality of life: Education, employment, and relationships:
- Education: Students with epilepsy might face challenges like memory issues or the need for frequent medical appointments. But did you ever consider the social aspect? The fear of having a seizure in class can be daunting.
- Employment: While many with epilepsy work full-time jobs, certain professions might be off-limits due to safety concerns. Moreover, the need for flexibility, especially around medical appointments or post-seizure recovery, is crucial.
- Relationships: Open communication is key. Partners, family, and friends play a pivotal role in offering emotional support and understanding the complexities of epilepsy.
2. Driving, safety, and first aid for seizures:
- Driving: Regulations vary by region, but many places require individuals to be seizure-free for a specific period before driving. But why? The unpredictability of seizures poses safety concerns.
- Safety: Simple measures, like avoiding swimming alone or using protective headgear, can make a difference.
- First Aid: Do you know what to do if someone has a seizure? Keeping the person safe, turning them to their side, and ensuring they're breathing are crucial steps. But remember, never place anything in their mouth during a seizure.
3. Coping mechanisms and mental health considerations:
Living with epilepsy can be emotionally taxing. Feelings of anxiety, depression, or isolation are not uncommon. So, how do individuals cope? Techniques like meditation, counseling, or simply joining a support group can offer solace and understanding.
4. Advocacy, support networks, and community resources:
The journey with epilepsy doesn't have to be a solitary one. Numerous organizations advocate for epilepsy awareness, research, and support. Connecting with these networks can provide resources, camaraderie, and a platform to shareexperiences.
Living with epilepsy is about more than managing seizures; it's about navigating the myriad challenges and joys of life with resilience and hope. This perspective prompts a thought: As society becomes more inclusive and understanding, how can we further support and uplift those living with epilepsy?
Epilepsy in Special Populations
Epilepsy doesn't discriminate, but its manifestation and management can vary across different age groups and genders. Let's delve into the unique challenges faced by these special populations.
1. Pediatric epilepsy: Unique challenges and management:
Children aren't just small adults. Their brains are still developing, and so the presentation and impact of epilepsy can be distinct. Challenges include ensuring accurate diagnosis (especially with seizures that might be mistaken for typical childhood behavior), managing side effects of medications on a growing body, and addressing the psychosocial impact on schooling and peer relationships. Tailored treatments, often involving a combination of medications and behavioral therapies, are crucial.
2. Epilepsy in the elderly:
As people age, the onset of epilepsy can be linked to other age-related conditions like stroke or Alzheimer's disease. Diagnosis can be tricky, with seizures sometimes mistaken for other neurological conditions. Additionally, the elderly might be on multiple medications, raising concerns about drug interactions. A careful, holistic approach to management is essential.
3. Women with epilepsy: Pregnancy and hormonal considerations:
For women with epilepsy, considerations extend beyond seizure management. Hormonal fluctuations during menstrual cycles can influence seizure patterns. And what about the desire to start a family? Pregnancy brings concerns about the effects of antiepileptic drugs on the fetus, and the potential for increased seizure frequency. Collaborative care involving neurologists and obstetricians is vital.
Future Directions and Innovations
The realm of epilepsy research is dynamic, with innovations promising better diagnostics, treatments, and perhaps even a cure.
1. Advances in genetic research and personalized medicine:
As we unravel the human genome, we're identifying genetic markers associated with certain types of epilepsy. This not only aids in diagnosis but also paves the way for personalized treatments tailored to an individual's genetic makeup.
2. Wearable technologies and seizure prediction:
Imagine if a wristband could warn you of an impending seizure. With advancements in wearable tech and data analytics, we're inching closer to real-time seizure prediction, allowing individuals to take precautions.
3. Potential for novel therapeutics and a cure
The quest for newer, more effective treatments is relentless. From exploring the potential of stem cells to harnessing the power of AI in drug discovery, the future holds immense promise. And with every research breakthrough, we edge closer to the ultimate goal: a cure.
Epilepsy, with its myriad facets, continues to be a focal point of medical research. As we look to the future, one can't help but wonder: In a world where we're pushing the boundaries of what's possible, how will our understanding and management of epilepsy evolve in the next decade?
Navigating the intricate maze of epilepsy, we've journeyed through its diverse presentations, the unique challenges faced by different demographics, and the promising horizon of research and innovation. But what does all this mean for the future of epilepsy care and for those living with the condition?
Epilepsy, once shrouded in mystery and misconceptions, has seen a transformative shift in understanding and management. With each passing decade, we've moved from rudimentary treatments to advanced diagnostic tools and personalized therapeutic strategies. The fusion of technology, genetics, and neuroscience promises a future where epilepsy care is not just about managing seizures but about enhancing the overall quality of life.
But beyond the realm of medicine and technology lies the human aspect. Living with epilepsy isn't just a clinical journey; it's a deeply personal one, intertwined with emotions, aspirations, and daily challenges. Recognizing this, there's a growing emphasis on holistic care that addresses not just the physical, but the emotional and psychosocial dimensions of the condition.
Moreover, societal support is paramount. From creating inclusive educational environments for children with epilepsy to fostering workplaces that understand and accommodate the needs of those with the condition, societal empathy and awareness can make a world of difference.
In closing, epilepsy, with its multifaceted challenges, also brings with it lessons of resilience, innovation, and community. As we continue to push the boundaries of what's possible in care and research, it's essential to remember that at the heart of it all is the individual – deserving of respect, understanding, and the best care that science and society can offer.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!





